| True Brown's syndrome is a stable, persistent limitation of eye elevation
in adduction. It is caused by a congenitally shortened and therefore
tight superior oblique muscle or tendon.31–33 In most cases, elevation in abduction is near normal, differentiating
Brown's syndrome from monocular elevation deficiency (double
elevator palsy). However, when the affected eye moves from abduction
to adduction, there may be a characteristic depression or downshoot. In
addition, in severe cases, the limitation may extend to primary
position, resulting in a hypotropia of the affected eye in primary gaze. Some
patients also may have increased amounts of abduction of the
affected eye on attempted elevation in primary position, resulting in
a Y pattern exotropia in upgaze. True Brown's syndrome must be distinguished from other simulating
conditions, such as inferior oblique palsy, monocular elevation deficiency (double
elevator palsy), paratrochlear trauma or inflammation
with resulting scarring and fibrosis, congenital periocular fibrous
bands, orbital floor fracture with entrapment of orbital contents, inferior
rectus fibrosis syndrome, mass effect from a glaucoma Seton
implant,34,35 and inferotemporal or posterior superonasal orbital fibrosis secondary
to the fat adherence syndrome that is associated with rupture of Tenon's
capsule and prolapse of fat during inferior oblique surgery. Exclusion
of these simulating conditions (pseudo-Brown's
syndrome) is important because most require a different management
approach. The diagnosis of true Brown's syndrome requires: (a) the
presence of typical clinical features described in the
preceding; (b) the presence of mechanical restriction to
elevation of the eye in adduction as demonstrated by forced duction testing
either before or during surgery; and (c) complete resolution
of all restriction after transection of the superior oblique tendon. Any
patient with suspected Brown's syndrome who does not meet
all three criteria should be evaluated thoroughly for alternative etiologies. INDICATIONS In true Brown's syndrome, surgical therapy is indicated for patients
with abnormal head posture, a hyperdeviation in primary position, or
diplopia. Most patients with Brown's syndrome have fusional ability; so
abnormal head posture is the most common indication for surgery. The
patient may have a chin-up posture to eliminate hypodeviation
in primary position or a face turn away from the affected eye, which
cannot adduct without depressing. The chronic head posturing can
result in musculoskeletal problems, difficulty with balance (especially
in young children), and cosmetic disfigurement. Diplopia
is an uncommon complaint in children who generally suppress the non-fixating
eye when a deviation is present, but it can be a problem
in previously well-compensated adults who later decompensate when
driving or when they become tired. Occasionally, adults with Brown's
syndrome complain of vague ocular discomfort characterized as
a pulling sensation or a sensation of ocular fatigue. However, by themselves, these
symptoms rarely are severe enough to indicate a need for
surgery. In addition, surgical correction sometimes should be considered
for occupational reasons in patients whose occupations (e.g., librarian, airline pilot, painter, or professional basketball player) have
significant upgaze requirements. Although immediate surgery is not necessary, children with mild to moderate
involvement without compensatory head posturing or vertical strabismus
in primary position need close observation and careful follow-up
for later development of the preceding surgical indications. Particular
attention should be given to documentation of the visual acuity
in each eye, the fusional and binocular status, and the presence of
even mild or intermittent degrees of head posturing. Evidence of loss
of binocularity, development of amblyopia, or loss of head posture suggests
decompensation with the development of suppression and a need
for immediate surgical correction. CONTRAINDICATIONS Many patients with Brown's syndrome have none of the preceding indications
and do not require surgery. They may have only minimal symptoms
or symptoms that are present only in extreme upgaze without head posture, or
they may report only unusual disconjugate eye movements in upgaze. Children
spend much of their time in upgaze looking at taller adults, which
accentuates even mild to moderate head posturing or disconjugate
eye movements. The marked secondary over-elevation of the
unaffected eye during upgaze may be the feature most readily observed
by parents, leading them to suspect an abnormality of the contralateral
normal eye. As a small child grows, the need for upgaze decreases, and
this sign becomes less noticeable. True Brown's syndrome is congenital; therefore, patients with unusual
features such as acute or acquired onset, the presence of pain or
active inflammation around the trochlea, or signs of any of the simulating
conditions listed in the preceding, require further evaluation before
surgery is considered. Some forms of acquired Brown's syndrome, such
as those with associated pain, other signs of inflammation, or
intermittency, respond to local corticosteroid injection. Other forms
may be an early manifestation of orbital tumors or localized subperiosteal
abscesses, and radiologic or sonographic imaging is needed for
proper diagnosis and treatment. In patients with acute traumatic Brown's
syndrome, which may occur after blunt orbital trauma or in canine
tooth syndrome, surgery should be deferred for at least 4 to 6 months
to determine whether spontaneous recovery occurs. PROCEDURES Superior Oblique Forced Duction Testing When any surgical procedure for suspected Brown's syndrome is performed, superior
oblique forced duction testing is required both preoperatively
and intraoperatively to confirm the diagnosis of true Brown's
syndrome and assess the adequacy of the surgical treatment. A simple
forced duction test is useful before surgery to confirm the diagnosis. The
globe is grasped with a toothed forceps at the limbus in the
inferotemporal quadrant. Taking care to maintain the globe in its proper
anterior-posterior position, the surgeon attempts to adduct
and elevate the eye into the superonasal quadrant. Tightness of the abnormally
short superior oblique muscle–tendon complex is easily
appreciated as the cause of the elevation limitation. Further confirmation
of the diagnosis is accomplished by demonstrating relatively free
range of motion into the superior temporal, inferior temporal, and inferior
nasal quadrants. A more sensitive technique, described by Guyton,36 is the exaggerated forced duction test. With this technique, the globe
is grasped near the limbus with a pair of forceps, at 3 and 9 o'clock, and
then maximally retro pulsed, extorted, elevated, and adducted
to place the superior oblique tendon on maximum stretch. Its tension
then can be felt by rocking the temporal forceps from inferior nasally
to superior temporally. As this maneuver is performed, the hand holding
the temporal forceps feels a tightening and loosening force as the
superior oblique tendon flips over the surface of the globe. With practice, the
degree of tightness of the superior oblique tendon can be
graded from normal to markedly increased, as in severe Brown's syndrome. The
exaggerated superior oblique forced duction test is valuable
immediately after every superior oblique tenotomy or other lengthening
procedure to verify that the entire tendon has been isolated and cut. The
presence of any residual flip requires a thorough search for residual
uncut tendon fibers. Alternatively, this residual action may indicate
the presence of posterior fibrous bands that restrict the globe
and must be sought and transected. It is likely that many cases of unsuccessful
surgery to correct Brown's syndrome are related to incomplete
transsection of all superior oblique tendon fibers, particularly
the most posterior ones that can be especially difficult to isolate. The
exaggerated superior oblique forced duction test should be performed
immediately after tenotomy to prevent this problem. Superior Oblique Weakening Procedures The abnormally short; therefore, a tight, superior oblique muscle–tendon
complex in Brown's syndrome can be lengthened (weakened) with
a number of techniques. As with other extraocular muscles, a
superior oblique tendon recession operation has been described.37 Theoretically this procedure can be performed in a graded fashion, as
shown in Figure 7, with larger amounts of recession for more severe restriction. In practice, however, several
technical problems compromise the effectiveness
and predictability of this operation. First, the broadly fanned, almost
diaphanous superior oblique insertion must be narrowed at the time
of recession so that it will hold a suture adequately. As shown in Figure 7, this
narrowed insertion is recessed a measured amount from the
original insertion (for small recessions) or reattached to the
sclera a measured distance from another reference point, such as the
nasal border of the superior rectus insertion, for larger recessions. Conversion
of the normal broad posterior lateral insertion, whose proximal
tendon slides easily over the nasal sclera, as the eye moves from
elevation to depression, to a narrow anterior nasal insertion fixed
to the sclera may convert the superior oblique from a strong depressor
and abductor to a weak elevator and adductor. The alteration in the
force vector thus created sometimes results in clinically significant
limitation of depression in the operated eye.32,36 This complication can be reduced by reattaching the recessed tendon more
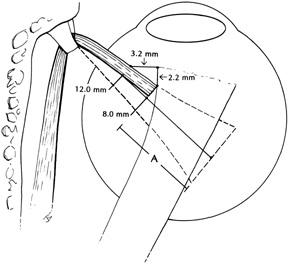
posteriorly on the globe.36 Because of these problems, the recession procedure is not widely used. 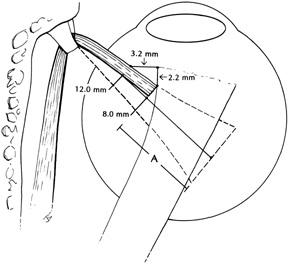 Fig. 7. Landmarks for quantitating superior oblique recession as described by Romano
and Roholt. The superior oblique tendon is secured with a double-armed 6-0 Vicryl suture and cut free from the sclera. This
narrowed insertion is then recessed a measured amount (A) from the original insertion. The distance can be measured directly for
small recessions (less than 6 mm). If it is recessed to a point 2.2 mm
posterior to the medial border of the superior rectus recession, the
net recession is 8 mm. If it is recessed to a point 3.2 mm
nasal to the nasal border of the superior rectus muscle, it is recessed 12 mm, as
shown. (Adapted from Romano P, Roholt P: Measured graduated
recession of the superior oblique muscle. J Pediatr Ophthalmol
Strabismus 20:136, 1983) Fig. 7. Landmarks for quantitating superior oblique recession as described by Romano
and Roholt. The superior oblique tendon is secured with a double-armed 6-0 Vicryl suture and cut free from the sclera. This
narrowed insertion is then recessed a measured amount (A) from the original insertion. The distance can be measured directly for
small recessions (less than 6 mm). If it is recessed to a point 2.2 mm
posterior to the medial border of the superior rectus recession, the
net recession is 8 mm. If it is recessed to a point 3.2 mm
nasal to the nasal border of the superior rectus muscle, it is recessed 12 mm, as
shown. (Adapted from Romano P, Roholt P: Measured graduated
recession of the superior oblique muscle. J Pediatr Ophthalmol
Strabismus 20:136, 1983)
|
Various other superior oblique weakening procedures have been proposed
to produce a weakening effect without complete tenotomy, with its potential
for late overcorrection and superior oblique palsy. Split tendon
lengthening at the insertion of the superior oblique tendon has been
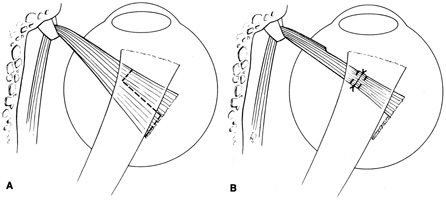
described.38 With this procedure, shown in Figure 8, the distal superior oblique tendon is separated into an anterior and
a posterior half for a specified length using a small muscle hook. The
tendon then is transected through the posterior half distally at the
insertion and through the anterior half at the proximal end of the split (Fig. 8A). The distal posterior hemitendon is sutured to
the proximal anterior hemitendon, as shown in Figure 8B, to lengthen the
tendon by an amount equal to the length of the anterior hemitendon. However, the
procedure requires extensive dissection of the intermuscular
septum surrounding the distal tendon, and it is technically difficult
to perform because of the wispy, diaphanous nature of the tendon
in this region.32 Some strabismus surgeons have found that extensive scarring of the floppy
distal tendon may make the procedure unpredictable in its initial
effect and variable in its long-term stability. However, recent
reports by Stolovitch and co-workers39 and Bardorf and Baker40 have suggested that this procedure can be used safely and effectively
for lengthening the superior oblique in selected patients with Brown's
syndrome. 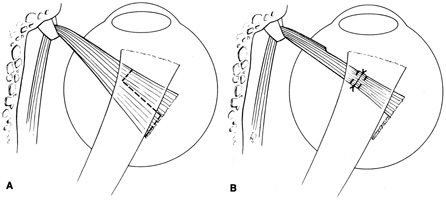 Fig. 8. Superior oblique weakening by split tendon lengthening. A. Incision lines (dashed lines) before the procedure is performed. B. Appearance after the procedure is completed. Fig. 8. Superior oblique weakening by split tendon lengthening. A. Incision lines (dashed lines) before the procedure is performed. B. Appearance after the procedure is completed.
|
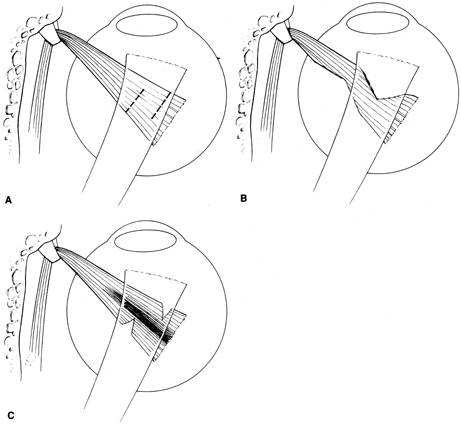
Another procedure, the Z-tenotomy of the distal superior oblique
tendon, is even less valuable as a superior oblique weakening procedure. The
Z-tenotomy, useful in weakening rectus muscles, lengthens
the tendon by adjacent two-thirds marginal tenotomies, as shown
in Figure 9A, one from the anterior tendon border and the other from the posterior
tendon border, that overlap in the center of the tendon. Theoretically, spreading
of these adjacent tenotomies elongates and loosens the tight
superior oblique tendon (Fig. 9B). However, unlike a Z-tenotomy
performed in muscle tissue, there is little cross-linking
force between longitudinal tendon fibers in the superior oblique
tendon. Therefore, the lengthened tendon tends to pull apart, converting
the Z-tenotomy into an inadvertent complete distal tenotomy. On
the other hand, if neither marginal tenotomy transects the central
longitudinal tendon fibers as shown in Figure 9C, no tendon lengthening
or weakening effect results. 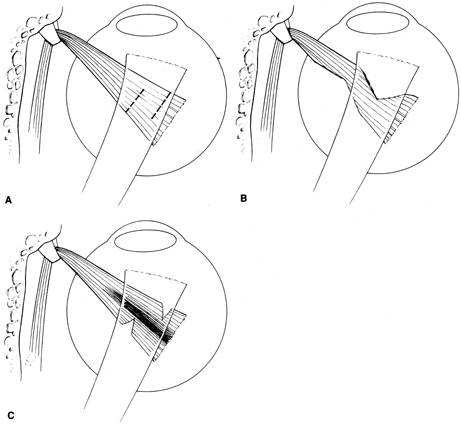 Fig. 9. Weakening of the superior oblique tendon by Z-tenotomy. A. The preoperative view shows the placement of incisions. Marginal tenotomies
must overlap centrally. B. The final result shows tendon lengthening. C. The result if neither marginal tenotomy transects the central longitudinal
tendon fibers, with no lengthening or weakening of the tendon. Fig. 9. Weakening of the superior oblique tendon by Z-tenotomy. A. The preoperative view shows the placement of incisions. Marginal tenotomies
must overlap centrally. B. The final result shows tendon lengthening. C. The result if neither marginal tenotomy transects the central longitudinal
tendon fibers, with no lengthening or weakening of the tendon.
|
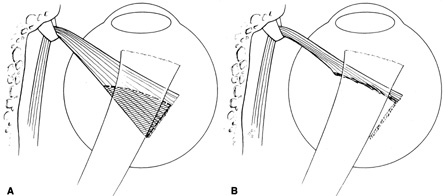
To reduce the risk of late overcorrection, two additional superior oblique
weakening procedures have been studied: superior oblique weakening
by a peripheral tenotomy near the tendon insertion and superior oblique
weakening by posterior two-thirds or seven-eighths tenectomy
at the insertion, as shown in Figure 10.41 However, in the authors' experience, these procedures (especially
the posterior seven-eighths tenectomy), although sometimes
effective in mild superior oblique overaction with A-pattern, often
produced unreliable and sometimes unstable results, especially
undercorrection or early recurrence. 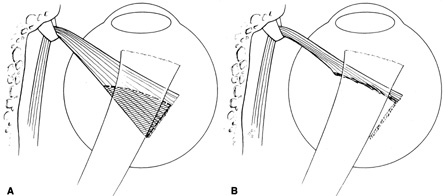 Fig. 10. Weakening of the superior oblique tendon by posterior tenectomy. A. The portion of the posterior tendon that will be resected (hatched
area) generally is three-fourths or seven-eighths
of the tendon width. B. The final result. The anterior fibers are maintained to prevent any torsional
effect. Fig. 10. Weakening of the superior oblique tendon by posterior tenectomy. A. The portion of the posterior tendon that will be resected (hatched
area) generally is three-fourths or seven-eighths
of the tendon width. B. The final result. The anterior fibers are maintained to prevent any torsional
effect.
|
Most strabismus surgeons now believe that the optimal surgical procedure
for correcting true Brown's syndrome involves complete tenotomy
or tenectomy of the superior oblique tendon nasal to the superior rectus
muscle border, either in an uncontrolled fashion or with the use of
a mechanical spacer to lengthen the cut ends of the tendon in a controlled
fashion. In 1946, Berke42 described a technique for complete tenotomy of the superior oblique tendon
nasal to the superior rectus muscle. He performed the procedure, which
consisted of blindly sweeping a muscle hook 10 to 12 mm posteriorly
through a superonasal conjunctival incision directly overlying the
nasal portion of the tendon. The hook then was swept superiorly to catch
the superior oblique tendon, but also surrounding Tenon's capsule
and orbital fat, which were later lifted off of the hook to identify
the tendon. A second report described three variations of this technique
to control the weakening effect.43 Berke recommended cutting the tendon just medial to the superior rectus
muscle if a minimal effect was desired.42 If a larger effect was desired, he performed a small tenectomy, but left
the surrounding “sheath” intact to allow some connection
between the cut end of the tendon and the globe. Complete superior oblique
palsy occurred if a portion of the tendon with its entire sheath
was excised close to the trochlea. Although isolated reports of superior
oblique tenotomy or tenectomy appeared after Berke's initial
description,44,45 Crawford was the first to report a large series comparing complete tenotomy
by the Berke technique with Z-tenotomy, split tendon lengthening, and
tenectomy. In his study, only tenotomy or tenectomy by the
Berke technique was completely effective.38 However, incomplete tenotomy or tenectomy, possibly owing to inadequate
visualization of the tendon before it was isolated with a muscle hook, resulted
in surgical failure on several occasions. Others also experienced
this difficulty with the use of the Berke technique.46 Parks47,48 subsequently developed an alternate technique to address some of the technical
problems he experienced with the Berke technique. A superior
temporal fornix incision is made through conjunctiva and Tenon's
capsule down to bare sclera, and the superior rectus is hooked through
this incision. The superior rectus then is exposed by reflecting the
intermuscular septum, Tenon's capsule, and conjunctiva over the toe
of the large hook. The nasal border of the superior rectus is exposed
by temporal traction on the muscle hook, securing the superior rectus
insertion while the conjunctival wound is further displaced nasally
with two Stevens muscle hooks or a Desmarres retractor. The superior
oblique tendon is identified visually as a cord of parallel fibers seen
coursing from beneath the nasal border of the superior rectus approximately 8 to 12 mm
posterior to its insertion. This technique allows isolation
of the superior oblique tendon under direct visualization. Once
isolated in this way, tenotomy or tenectomy of the tendon can be completed
with almost no violation of surrounding intermuscular septum or
Tenon's capsule. Therefore, once the tendon is cut, the cut ends
separate but maintain their normal anatomic relationships. Because they
are still embedded in intermuscular septum and surrounding Tenon's
tissue, they continue to provide a weakened but vectorially normal
force on the globe, thereby reducing the incidence of consecutive superior
oblique palsy.49 At the completion of the procedure, all instruments are removed from the
eye. The exaggerated forced duction test is repeated to verify that
all superior oblique tendon fibers have been transected. The advantages of the Parks technique over others described include: (a) direct
visualization of the entire tendon before isolation
with the muscle hook, thereby eliminating the riskier blind hooking of
the tendon, with its increased risk of incomplete tendon isolation, violation
of the orbital fat, or inadvertent transection of the superior
rectus muscle;50 (b) transection of the cordlike tendon nasal to the superior
rectus, where the weakening effect is more predictable; and (c) transection
with minimal or no dissection of surrounding intermuscular
septum, thereby preventing uncontrolled scarring with reattachment
of the superior oblique tendon to the sclera in an unwanted location, or
alteration of the tendon's course, which might change its vector
of action on the globe. A modification of the Park's technique, preferred
by the authors, is described in the following.49 Additional information about the superior oblique tenotomy or tenectomy
technique is provided in another chapter. Superior Oblique Tenotomy Performed on the Right Superior Oblique Tendon Step 1. With the eye depressed and adducted by the assistant, a superior-temporal, two-plane fornix incision is made approximately 8 mm
posterior to the limbus. It is important to keep the incision parallel
to the upper lid so that the upper lid will cover the closed wound
at the end of the procedure.
Step 2. The temporal border of the superior rectus is then isolated through the
incision, first with a small Stevens muscle hook and then with a larger
Green or Jameson muscle hook to provide adequate control of the globe.
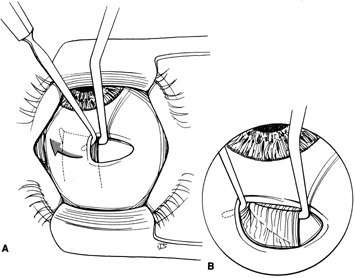
Step 3. Although traction is applied on the superior rectus with the large muscle
hook to depress the globe, a Stevens hook held in the other hand is
used to expose the superior rectus insertion by reflecting the intermuscular
septum, Tenon's capsule, and conjunctiva over the toe of
the large hook as shown in Figures 11A (before reflection) and 11B (after reflection).
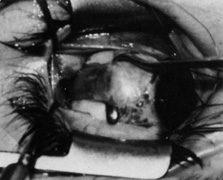
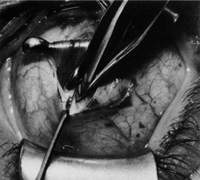
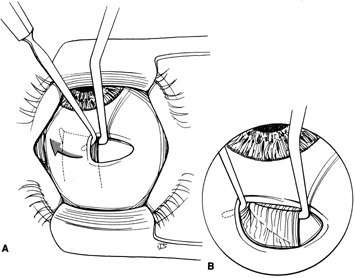 Fig. 11. A. Traction on the superior rectus muscle with the large muscle hook is applied
to depress the globe. B. A Stevens hook held in the other hand is used to expose the superior rectus
insertion by reflecting the intermuscular septum, Tenon's capsule, and
conjunctiva over the toe of the hook. (Del Monte MA, Archer
SM: Atlas of Pediatric Ophthalmology and Strabismus Surgery. New
York: Churchill Livingstone, 1993) Fig. 11. A. Traction on the superior rectus muscle with the large muscle hook is applied
to depress the globe. B. A Stevens hook held in the other hand is used to expose the superior rectus
insertion by reflecting the intermuscular septum, Tenon's capsule, and
conjunctiva over the toe of the hook. (Del Monte MA, Archer
SM: Atlas of Pediatric Ophthalmology and Strabismus Surgery. New
York: Churchill Livingstone, 1993)
|
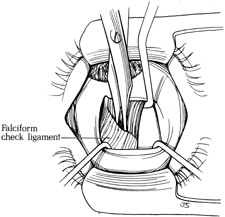
Step 4. With the eye maximally depressed with the Green hook beneath the superior
rectus, the superior surface of the superior rectus is exposed with
two Stevens hooks, as shown in Figure 12. This maneuver exposes the broad, sheetlike white falciform check ligament
that fuses to the superior rectus diagonally 8 to 12 mm posterior
to its insertion. The ligament is opened centrally at its insertion with
blunt Westcott scissors.
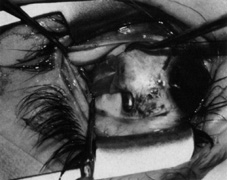
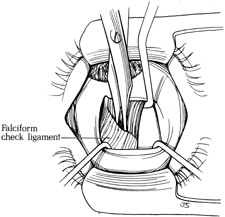 Fig. 12. With the eye maximally depressed with the Green hook beneath the superior
rectus muscle, the superior surface of the muscle is exposed with two
Stevens hooks. The broad, sheet-like white falciform check ligament
is exposed. This ligament fuses to the superior rectus muscle
diagonally 8 to 12 mm posterior to its insertion. The ligament is opened
centrally at its insertion with blunt Westcott scissors. (Del
Monte MA, Archer SM: Atlas of Pediatric Ophthalmology and Strabismus Surgery. New
York: Churchill Livingstone, 1993) Fig. 12. With the eye maximally depressed with the Green hook beneath the superior
rectus muscle, the superior surface of the muscle is exposed with two
Stevens hooks. The broad, sheet-like white falciform check ligament
is exposed. This ligament fuses to the superior rectus muscle
diagonally 8 to 12 mm posterior to its insertion. The ligament is opened
centrally at its insertion with blunt Westcott scissors. (Del
Monte MA, Archer SM: Atlas of Pediatric Ophthalmology and Strabismus Surgery. New
York: Churchill Livingstone, 1993)
|
Step 5. Two Stevens hooks are used to enlarge the opening in the check ligament
and expose the bare superior surface of the superior rectus muscle posteriorly. A
Desmarres retractor is inserted through this opening to
further retract Tenon's capsule exposing the nasal border of the
superior rectus.
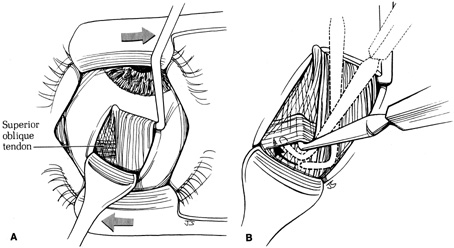
Step 6. To improve visualization of the nasal border of the superior rectus, the
Green muscle hook under the superior rectus is pulled temporally and
the Desmarres retractor moved nasally. This maneuver exposes the untouched
wispy nasal intermuscular septum that covers and encases the parallel
fibers of the superior oblique tendon (Fig. 13A) as they pass beneath the superior rectus muscle. In some patients, exposure
of the tendon can be improved at this time by removing the
lid speculum, allowing greater retraction with the Desmarres retractor.
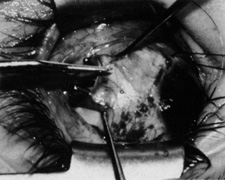
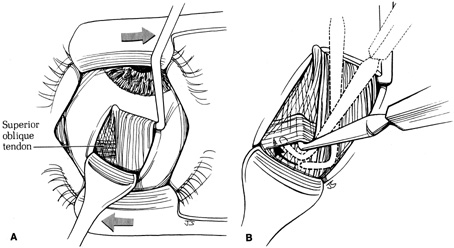 Fig. 13. A. The Green muscle hook under the superior rectus muscle is pulled temporally
and a Desmarres retractor moved nasally to improve visualization
of the nasal border of the muscle. This maneuver exposes the nasal intermuscular
septum, which covers and encases the parallel fibers of the
superior oblique tendon as they pass beneath the superior rectus muscle. B. A Stevens muscle hook, with its tip pointing nasally, is moved posteriorly
along the nasal border of the superior rectus muscle until the posterior
margin of the cordlike superior oblique tendon is clearly identified. The
tip of the hook is rotated posteriorly behind the tendon and
passed toward the sclera anteriorly beneath the superior oblique tendon. (Del
Monte MA, Archer SM: Atlas of Pediatric Ophthalmology
and Strabismus Surgery. New York: Churchill Livingstone, 1993) Fig. 13. A. The Green muscle hook under the superior rectus muscle is pulled temporally
and a Desmarres retractor moved nasally to improve visualization
of the nasal border of the muscle. This maneuver exposes the nasal intermuscular
septum, which covers and encases the parallel fibers of the
superior oblique tendon as they pass beneath the superior rectus muscle. B. A Stevens muscle hook, with its tip pointing nasally, is moved posteriorly
along the nasal border of the superior rectus muscle until the posterior
margin of the cordlike superior oblique tendon is clearly identified. The
tip of the hook is rotated posteriorly behind the tendon and
passed toward the sclera anteriorly beneath the superior oblique tendon. (Del
Monte MA, Archer SM: Atlas of Pediatric Ophthalmology
and Strabismus Surgery. New York: Churchill Livingstone, 1993)
|
Step 7. A Stevens muscle hook, with its tip pointing nasally, is moved posteriorly
along the nasal border of the superior rectus muscle until the posterior
margin of the cordlike superior oblique tendon is clearly identified. The
tip of the hook is then rotated posteriorly behind the tendon
and passed toward the sclera and anteriorly beneath the superior oblique
tendon, pushing the intermuscular septum behind the tendon to surround
it completely, as shown in Figure 13B.
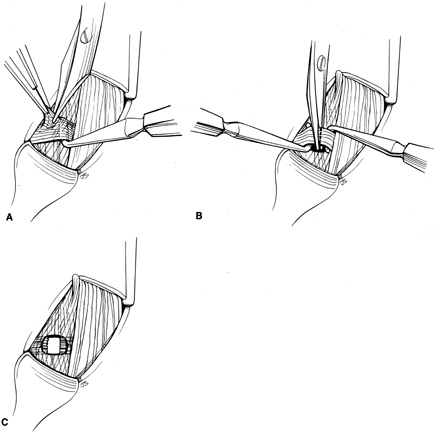
Step 8. The two layers of intermuscular septum on the toe of the Stevens hook
are opened anterior to the tendon with a blunt Westcott scissors, as shown
in Figure 14A. A second Stevens hook is passed through the anterior opening in intermuscular
septum and beneath the tendon from anterior to posterior. These
two Stevens hooks, passing beneath the tendon in opposite directions, securely
hold the tendon in place until the tenotomy is completed. The
tenotomy is performed between them with blunt Westcott scissors, as
shown in Figure 14B, with care taken not to damage adjacent intermuscular
septum. The opposite pointing Stevens hooks hold the tendon securely
until it is completely transected and the hooks are released.
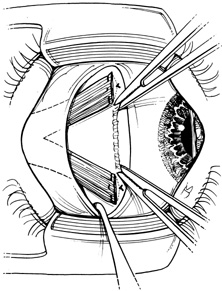
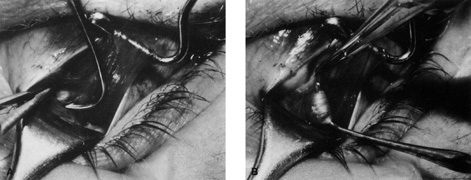
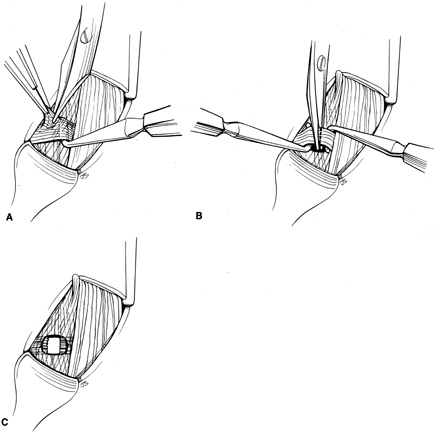 Fig. 14. A. The two layers of intermuscular septum on the toe of the Stevens hook
are opened anterior to the tendon with blunt Westcott scissors. B. A second Stevens hook is passed through the anterior opening of the intermuscular
septum and beneath the tendon from anterior to posterior. The
tenotomy is performed between them with blunt Westcott scissors. Care
is taken to avoid damaging the adjacent intermuscular septum. C. The cut ends of the tendon are visualized as they lie separated within
the small rent in the intermuscular septum nasal to the superior rectus
muscle. (Del Monte MA, Archer SM: Atlas of Pediatric Ophthalmology
and Strabismus Surgery. New York: Churchill Livingstone, 1993) Fig. 14. A. The two layers of intermuscular septum on the toe of the Stevens hook
are opened anterior to the tendon with blunt Westcott scissors. B. A second Stevens hook is passed through the anterior opening of the intermuscular
septum and beneath the tendon from anterior to posterior. The
tenotomy is performed between them with blunt Westcott scissors. Care
is taken to avoid damaging the adjacent intermuscular septum. C. The cut ends of the tendon are visualized as they lie separated within
the small rent in the intermuscular septum nasal to the superior rectus
muscle. (Del Monte MA, Archer SM: Atlas of Pediatric Ophthalmology
and Strabismus Surgery. New York: Churchill Livingstone, 1993)
|
Step 9. The cut ends of the tendon are visualized as they lie separated, exposed
within the rent in the intermuscular septum nasal to the superior rectus
muscle, as shown in Figure 14C. If the tendon is particularly tight, the
nasal end may retract out of sight toward the trochlea, along
its normal course through intermuscular septum.
Step 10. All instruments are removed from the incision, and the superior temporal
conjunctival wound is massaged closed into the fornix. The surgeon
must then verify that the tenotomy is complete by repeating the exaggerated
forced duction test described in the preceding. In a complete tenotomy, no
superior oblique tightness should be felt. Any residual tension, even
mild, suggests that the tenotomy is incomplete. In that case, the
Green hook must be replaced beneath the superior rectus and a Desmarres
retractor repositioned to expose the nasal border of the superior
rectus muscle. A thorough visual and physical search for residual
uncut posterior tendon fibers can then be made with a Stevens hook. Only
when the forced ductions are completely negative can the surgeon be
certain that complete tenotomy has been accomplished. This confirmation
is important because even a few remaining uncut fibers will prevent
any surgical weakening effect.
Superior Oblique Tendon Silicone Expander Procedure Recently, Wright and associates51–53 described a new technique for correcting superior oblique overaction and
Brown's syndrome by performing a superior oblique tenotomy and
inserting a measured spacer of #240 or #40 silicone retinal band
securely between the cut ends of the tendon. The degree of lengthening
can be controlled by the length of silicone band inserted, with a
longer band inserted to correct a greater restriction. Forced duction
testing after insertion will verify the proper weakening effect. The
presumed advantage of the silicone expander technique over uncontrolled
tenotomy is that the expander prevents the excessive lengthening of
the tendon that can result in superior oblique palsy.51 In addition, the expander lengthens the tendon without altering the location
or functional characteristics of the broadly fanned posterior insertion. The
use of a silicone band has a theoretical advantage over
the use of sutures or other flexible spacers because the silicone band
retains its length after healing and prevent scar contraction from reducing
the tendon separation and causing recurrence of the Brown's
syndrome.51 When performed properly, with exposure of the tendon using the Parks superior
oblique tenotomy technique and careful removal of the tendon from
its capsule before transection, the silicone expander retracts into
the tendon capsule at the end of the procedure without scarring surrounding
tissues or underlying sclera. Superior Oblique Silicone Tendon Expander Procedure Performed on the Right
Superior Oblique Tendon Step 1. A Jameson hook is placed beneath the superior rectus muscle through a
superior-temporal fornix incision, and the conjunctiva and Tenon's
capsule are reflected over the superior rectus insertion with
a Stevens hook. This maneuver exposes the distal superior rectus with
the adherent broad sheetlike white check ligament that fuses to its superior
surface diagonally 8 to 12 mm posterior to its insertion. The
ligament is opened centrally at its insertion on the surface of the superior
rectus with blunt Westcott scissors, as shown in Figure 15.
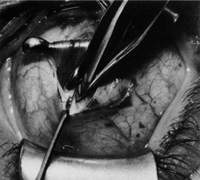 Fig. 15. A Jameson hook is placed beneath the superior rectus muscle through a superior
temporal fornix incision. The conjunctiva and Tenon's capsule
are reflected over the superior rectus insertion with a Stevens hook. This
maneuver exposes the distal superior rectus muscle, with its
adherent broad sheet like check ligament fusing to its superior surface
diagonally 8 to 12 mm posterior to its insertion. The ligament is opened
centrally at its insertion on the surface of the superior rectus
muscle with blunt Westcott scissors. Fig. 15. A Jameson hook is placed beneath the superior rectus muscle through a superior
temporal fornix incision. The conjunctiva and Tenon's capsule
are reflected over the superior rectus insertion with a Stevens hook. This
maneuver exposes the distal superior rectus muscle, with its
adherent broad sheet like check ligament fusing to its superior surface
diagonally 8 to 12 mm posterior to its insertion. The ligament is opened
centrally at its insertion on the surface of the superior rectus
muscle with blunt Westcott scissors.
|
Step 2. Two Stevens hooks are used to enlarge the opening in the check ligament, exposing
the bare superior surface of the superior rectus muscle posteriorly. A
Desmarres retractor is inserted through this opening to further
retract Tenon's capsule and expose the nasal border of the
superior rectus muscle, allowing direct visualization of the underlying
parallel cordlike fibers of the superior oblique tendon (Fig. 16). Visualization can be improved by removing the lid speculum and
by moving the Jameson hook beneath the superior rectus temporally and
the Desmarres retractor nasally, as shown in Figure 16.
 Fig. 16. Two Stevens hooks are used to enlarge the opening in the check ligament, exposing
the bare superior surface of the superior rectus muscle posteriorly. A
Desmarres retractor is inserted through this opening to further
attract Tenon's capsule and expose the nasal border of the
superior rectus muscle, allowing direct visualization of the underlying
parallel cordlike fibers of the superior oblique tendon (arrow). A small incision is made through the wispy capsule overlying the superior
oblique tendon to bare the tendon fibers. Fig. 16. Two Stevens hooks are used to enlarge the opening in the check ligament, exposing
the bare superior surface of the superior rectus muscle posteriorly. A
Desmarres retractor is inserted through this opening to further
attract Tenon's capsule and expose the nasal border of the
superior rectus muscle, allowing direct visualization of the underlying
parallel cordlike fibers of the superior oblique tendon (arrow). A small incision is made through the wispy capsule overlying the superior
oblique tendon to bare the tendon fibers.
|
Step 3. A small incision is made through the wispy capsule overlying the superior
oblique tendon to bare the tendon fibers. It is important to avoid
incising surrounding intermuscular septum, as shown in Figure 16.
Step 4. The exposed superior oblique tendon is engaged with a Stevens hook through
the small hole in the superior oblique tendon capsule (Fig. 17A), with care taken not to rupture the posterior capsule and expose
bare sclera (Fig. 17B). Any remaining adherent fascia or tendon
capsule is removed carefully with a 0.3 Castroviejo forceps, as shown.
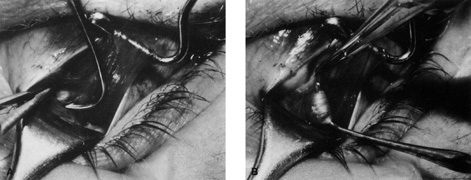 Fig. 17. A. The exposed superior oblique tendon is engaged with a Stevens hook through
the small hole in the superior oblique tendon capsule. B. The entire tendon is secured on the Stevens hook, where adherent fascia
and intermuscular septum are removed with a 0.3-mm Castroviejo
forceps. Fig. 17. A. The exposed superior oblique tendon is engaged with a Stevens hook through
the small hole in the superior oblique tendon capsule. B. The entire tendon is secured on the Stevens hook, where adherent fascia
and intermuscular septum are removed with a 0.3-mm Castroviejo
forceps.
|
Step 5. A second Stevens hook is placed beneath the tendon, and the exposed segment
is lifted out of its capsule. The tendon is secured with two double-armed 5-0 or 6-0 Mersilene (Ethicon, Somerville, NJ) sutures
with spatulated needles or 6-0 Ethibond
sutures with tapered vascular needles, one 2 to 3 mm nasal to the superior
rectus border and the other 2 to 3 mm nasal to the first suture, as
shown in Figure 18. Each suture is secured by a full-width, half-thickness
pass through the tendon, with locking bites placed on each edge and both
arms tied together in a square knot on the tendon surface, as shown
in Figure 18.
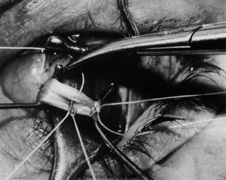
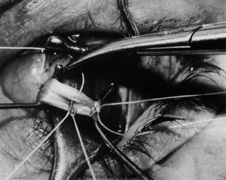 Fig. 18. A second Stevens hook is placed beneath the tendon, and the exposed segment
is lifted out of its capsule. The tendon is secured with two double-armed 5-0 or 6-0 Mersilene sutures with spatulated
needles, one 1- to 3-mm nasal to the superior rectus
muscle border and the other 2- to 3-mm nasal to the first
suture. Each is secured by a full-tendon, half-thickness
pass through the tendon, with locking bites placed on each edge and
both arms tied together in a square knot on the tendon surface. Fig. 18. A second Stevens hook is placed beneath the tendon, and the exposed segment
is lifted out of its capsule. The tendon is secured with two double-armed 5-0 or 6-0 Mersilene sutures with spatulated
needles, one 1- to 3-mm nasal to the superior rectus
muscle border and the other 2- to 3-mm nasal to the first
suture. Each is secured by a full-tendon, half-thickness
pass through the tendon, with locking bites placed on each edge and
both arms tied together in a square knot on the tendon surface.
|
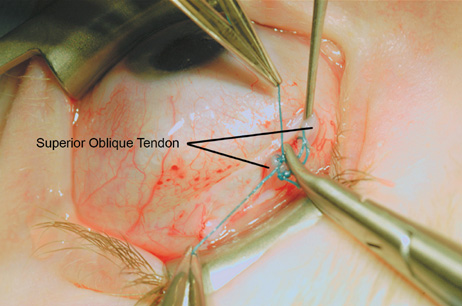
Step 6. The tendon is transected between the two pre-placed sutures, as
shown in Figure 19. The cut proximal tendon end will retract into its capsule, allowing inspection
of the opened tendon capsule for any defects. Large defects
discovered at this time can be closed with 6-0 Vicryl (Ethicon, Somerville, NJ) suture to prevent adherence of the tendon or
expander to the sclera postoperatively.
 Fig. 19. The superior oblique tendon is transected between the two preplaced sutures. Fig. 19. The superior oblique tendon is transected between the two preplaced sutures.
|
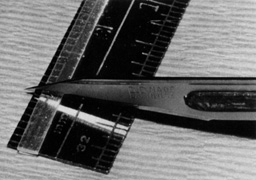
Step 7. A segment of a 240 silicone retinal band that has been previously soaked
in antibiotic solution is cut to the proper length with a #11 Beaver
blade and surgical ruler, as shown in Figure 20. The proper length that is needed to release the restriction without compromise
of superior oblique function can be determined by experience
based on the amount of forced duction tightness. A 7- to 8-mm
segment of band can be used initially in moderate to severe Brown's
syndrome, with the proper length of expander verified by forced
duction testing after insertion.
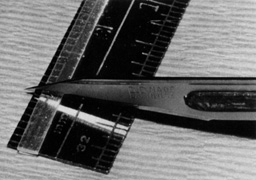 Fig. 20. A segment of #240 silicone retinal band is cut to the proper length
with a #11 Beaver blade. The proper length can be determined by experience
based on the tightness on forced duction testing. A 7- to 8-mm
segment of band can be used initially in moderate to
severe Brown's syndrome, with the proper length of expander verified
by forced duction testing after insertion. Fig. 20. A segment of #240 silicone retinal band is cut to the proper length
with a #11 Beaver blade. The proper length can be determined by experience
based on the tightness on forced duction testing. A 7- to 8-mm
segment of band can be used initially in moderate to
severe Brown's syndrome, with the proper length of expander verified
by forced duction testing after insertion.
|
Step 8. The double-armed Mersilene sutures from the cut ends of the tendon
are then secured to the ends of the silicone band in mattress fashion, as
shown in Figure 21. The sutures are pulled up to position the silicone band tightly against
the cut ends of the tendon. The double-armed sutures are then
tied together, and the suture ends trimmed (Fig. 22).
 Fig. 21. The double-armed Mersilene sutures from the cut ends of the tendon
are secured to the ends of the silicone band in mattress fashion. Fig. 21. The double-armed Mersilene sutures from the cut ends of the tendon
are secured to the ends of the silicone band in mattress fashion.
|
 Fig. 22. The sutures are pulled up to position the silicone band tightly against
the ends of the tendon. Then, the double-armed sutures are tied
together, and the suture ends trimmed. Fig. 22. The sutures are pulled up to position the silicone band tightly against
the ends of the tendon. Then, the double-armed sutures are tied
together, and the suture ends trimmed.
|
Step 9. When the sutures and expander are released, the proximal tendon retracts
and frequently pulls most, if not all, of the expander into the intact
proximal tendon capsule, as shown in Figure 23, leaving little, if any, expander exposed. The small opening in the tendon
capsule is closed with 6-0 plain gut suture to completely
isolate the cut tendon ends and silicone expander within the tendon capsule
to prevent scarring to surrounding sclera, orbital fat, superior
rectus muscle, or overlying conjunctiva. All instruments are removed, and
the conjunctival incision is massaged closed in the superior temporal
quadrant.
 Fig. 23. When the sutures and expander are released, the proximal tendon retracts. Frequently, it
pulls most, if not all, of the expander into the intact
proximal tendon capsule, as shown. A short segment of expander is
still exposed (arrow). Then, the small opening in the tendon capsule is carefully closed with 6-0 plain
gut sutures to completely isolate the cut tendon ends
and the expander within the tendon capsule. Fig. 23. When the sutures and expander are released, the proximal tendon retracts. Frequently, it
pulls most, if not all, of the expander into the intact
proximal tendon capsule, as shown. A short segment of expander is
still exposed (arrow). Then, the small opening in the tendon capsule is carefully closed with 6-0 plain
gut sutures to completely isolate the cut tendon ends
and the expander within the tendon capsule.
|
Step 10. Finally, standard (not exaggerated) superior oblique forced
duction testing should be performed, as shown in Figure 24. If the superior oblique restriction has not been relieved, the silicone
expander should be replaced with a longer one, and forced duction testing
repeated.
 Fig. 24. Standard (not exaggerated) superior oblique forced duction testing
is performed. The globe is grasped near the limbus in the inferotemporal
quadrant and rotated superiorly and nasally to verify that superior
oblique restriction has been relieved. The inferior limbus should
move well above an imaginary line connecting the medial and lateral
canthus. Fig. 24. Standard (not exaggerated) superior oblique forced duction testing
is performed. The globe is grasped near the limbus in the inferotemporal
quadrant and rotated superiorly and nasally to verify that superior
oblique restriction has been relieved. The inferior limbus should
move well above an imaginary line connecting the medial and lateral
canthus.
|
Suture Guarded Superior Oblique Tenotomy via the Temporal Approach An alternative procedure to the superior oblique expander procedure is
the suture guarded superior oblique tenotomy. This procedure shares many
advantages with the silicone expander over uncontrolled tenotomy in
that it is a graded procedure so the degree of tendon lengthening can
be controlled by the length of the suture separating the cut ends of
the tendon. In addition, a potential advantage of the suture-guarded
tenotomy over the silicone spacer procedure is the smaller size
of the suture material and the lower likelihood for extrusion or encapsulation
in dense scar tissue. The following steps outline the authors' approach to a temporal guarded
tenotomy of the left superior oblique from the surgeon's view (feet
toward the top and head toward the bottom): Step 1. After appropriate forced duction testing, the eye is depressed and adducted
by the assistant and a superior temporal, two-plane fornix
incision is made through conjunctiva and Tenon's capsule approximately 8 mm
posterior to the limbus.
Step 2. The superior rectus muscle is isolated through the incision first with
a small Stevens hook, and then with a larger Green or Jameson hook.
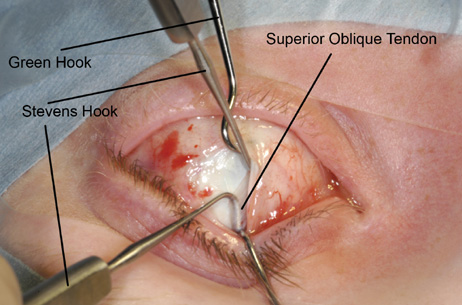
Step 3. While inferior traction is applied to the superior rectus with the large
muscle hook, the lid speculum is removed and another Stevens hook is
inserted into the wound to aid in exposure and visualization, exposing
the parallel white fibers of the superior oblique tendon running beneath
the superior rectus muscle, approximately 8 mm posterior to the
superior rectus insertion (Fig. 25).
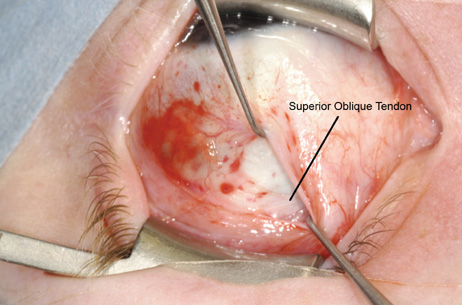 Fig. 25. Although inferior traction is applied to the superior rectus with the large
muscle hook, the lid speculum is removed and another Stevens hook
is inserted into the wound to aid in exposure and visualization, exposing
the parallel white fibers of the superior oblique tendon running
beneath the superior rectus muscle, approximately 8 mm posterior to the
superior rectus insertion. Fig. 25. Although inferior traction is applied to the superior rectus with the large
muscle hook, the lid speculum is removed and another Stevens hook
is inserted into the wound to aid in exposure and visualization, exposing
the parallel white fibers of the superior oblique tendon running
beneath the superior rectus muscle, approximately 8 mm posterior to the
superior rectus insertion.
|
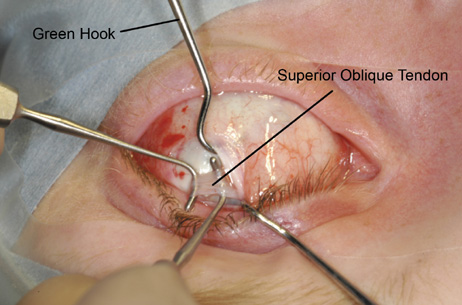
Step 4. Once the superior oblique tendon is visualized, a second Stevens hook, with
its tip pointed posteriorly, is used to engage the anterior fibers
of the superior oblique tendon (Fig. 26). The engaged fibers on the Stevens hook then are pulled temporally, exposing
the more fusiform portion of the tendon that normally lies
nasal to the superior rectus. This maneuver allows direct visualization
of the entire anterior and posterior borders of the tendon. Once this
fusiform portion of the tendon is directly visualized, it can be safely
isolated with a Stevens hook. The Stevens hook, with its tip nasally, is
moved posteriorly along the temporal border of the superior rectus
muscle until the posterior margin of the superior oblique tendon
is identified. The tip of the hook then is rotated inferiorly behind
the tendon, and then passed anteriorly beneath the tendon.
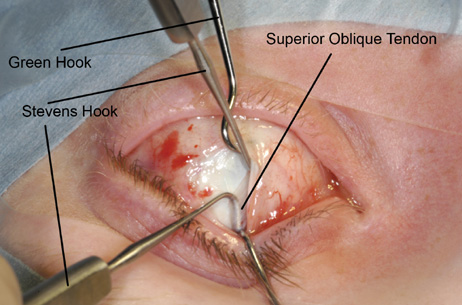 Fig. 26. Once the superior oblique tendon is visualized more fully with the help
of another Stevens hook to pull the superior rectus nasally, a second
Stevens hook, with its tip pointed posteriorly, is used to engage the
anterior fibers of the superior oblique tendon. Fig. 26. Once the superior oblique tendon is visualized more fully with the help
of another Stevens hook to pull the superior rectus nasally, a second
Stevens hook, with its tip pointed posteriorly, is used to engage the
anterior fibers of the superior oblique tendon.
|
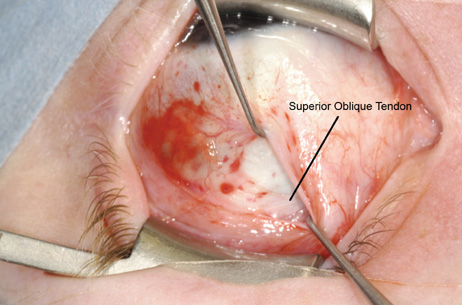
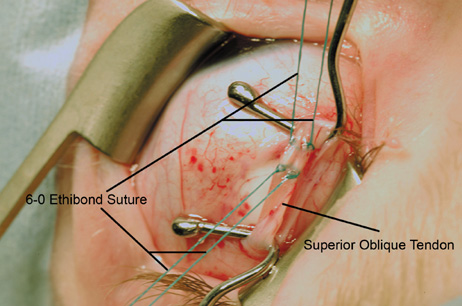
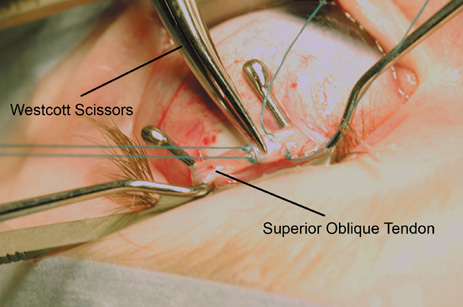
Step 5. A second Stevens hook is placed beneath the tendon, and the exposed segment
is lifted out of the capsule (Fig. 27). The tendon is secured with two doubled armed 6-0 Ethibond
sutures with tapered vascular needles, one 2 to 3 mm temporal to the
temporal border of the superior rectus, and the other 2 to 3 mm temporal
to the first. Each suture is secured by a full width, half-thickness
pass through the tendon, with locking bites at either end (Fig. 28).
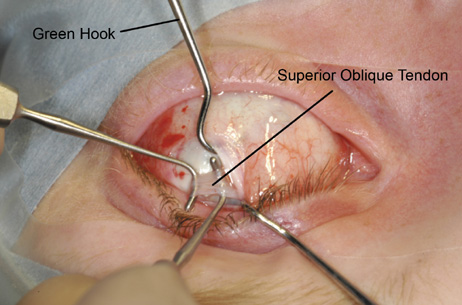 Fig. 27. With infraduction maintained by a Green Hook beneath the superior rectus, a
second Stevens hook is placed beneath the tendon, and the exposed
segment is lifted out of the capsule and away from the sclera. Fig. 27. With infraduction maintained by a Green Hook beneath the superior rectus, a
second Stevens hook is placed beneath the tendon, and the exposed
segment is lifted out of the capsule and away from the sclera.
|
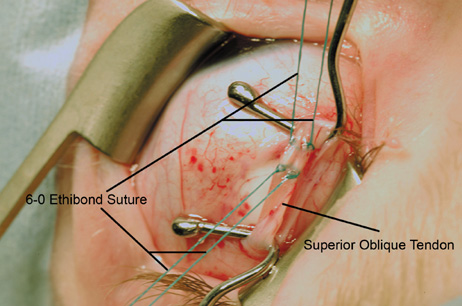 Fig. 28. The tendon is secured with two doubled-armed 6-0 Ethibond
sutures with tapered vascular needles, one 2 to 3 mm temporal to the
temporal border of the superior rectus, and the other 2 to 3 mm temporal
to the first. Each suture is secured by a full width, half-thickness
pass through the tendon, with locking bites at either end. Fig. 28. The tendon is secured with two doubled-armed 6-0 Ethibond
sutures with tapered vascular needles, one 2 to 3 mm temporal to the
temporal border of the superior rectus, and the other 2 to 3 mm temporal
to the first. Each suture is secured by a full width, half-thickness
pass through the tendon, with locking bites at either end.
|
Step 6. The tendon is transected between the two pre-placed sutures (Fig. 29).
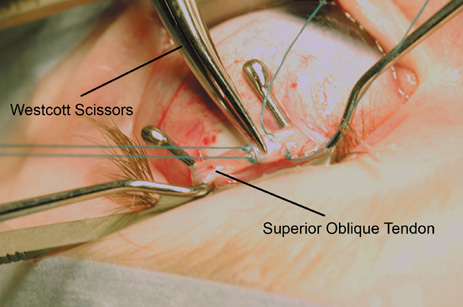 Fig. 29. The tendon is transected between the two preplaced sutures with a blunt
Westcott scissors. Fig. 29. The tendon is transected between the two preplaced sutures with a blunt
Westcott scissors.
|
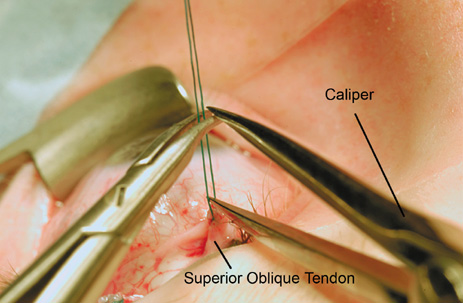
Step 7. Calipers set at desired amount of tendon lengthening (initially try 7 to 8 mm
for a moderate to severe Brown's syndrome) are
used to measure this distance from the proximally cut end of the tendon
along the double-armed suture. A straight or curved needle driver
is used to cross-clamp the two ends of the suture at this
measured point (Fig. 30).
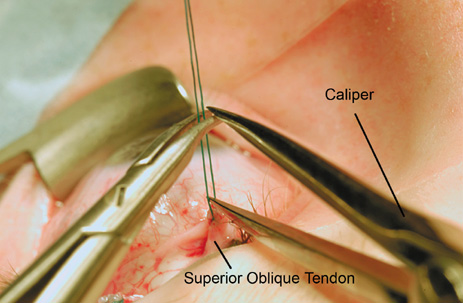 Fig. 30. Calipers set at desired amount of tendon lengthening (initially try 7 to 8 mm
for a moderate to severe Brown syndrome) are used to
measure this distance from the proximally cut end of the tendon along
the double-armed suture. A curved needle driver is used to clamp
the two ends of the suture at this measured point. Fig. 30. Calipers set at desired amount of tendon lengthening (initially try 7 to 8 mm
for a moderate to severe Brown syndrome) are used to
measure this distance from the proximally cut end of the tendon along
the double-armed suture. A curved needle driver is used to clamp
the two ends of the suture at this measured point.
|
Step 8. The two double-armed sutures are then sutured together (superior
arm to superior arm; inferior arm to inferior arm) at the
point marked by the needle driver, taking care to bring the knots as close
to the needle driver as possible (Fig. 31).
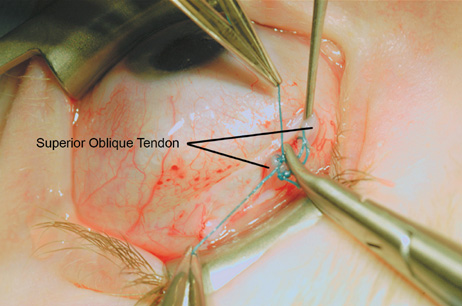 Fig. 31. The two double-armed sutures are then sutured together (superior
arm to superior arm; inferior arm to inferior arm) at the point
marked by the needle driver, taking care to bring the knots as close
to the needle driver as possible. Fig. 31. The two double-armed sutures are then sutured together (superior
arm to superior arm; inferior arm to inferior arm) at the point
marked by the needle driver, taking care to bring the knots as close
to the needle driver as possible.
|
Step 9. The suture ends are cut, and the needle driver is released, allowing the
cut tendon ends to separate by the measured suture length. When the
needle driver is released, the proximal tendon retracts beneath the temporal
border of the superior rectus.
Step 10. All instruments are removed from the eye and standard forced duction testing
is performed. If the superior oblique restriction has not been
relieved, the sutures can be replaced with a longer measured segment of
suture in the same manner.
Step 11. Once adequate forced ductions are confirmed, the superior-temporal
incision is massaged closed with a Stevens hook.
EXPECTED RESULTS The goals of therapy for Brown's syndrome include: (a) elimination
of abnormal head posturing, (b) normalization of
ductions and versions, and (c) functional improvement in fusional
status in important fields of gaze. Initial therapy, based on the
incorrect assumption that Brown's syndrome was caused by a shortening
or contracting of the sheath surrounding the superior oblique tendon, consisted
of lysis or stripping of the sheath. The results of studies
in which this technique was used were poor.54,55 Brown56 reported poor results in 36 patients treated with sheathotomy, sometimes
associated with an ipsilateral inferior oblique tuck or a superior
rectus recession. Only five of 36 showed significant improvement. Results
reported by others were even more disappointing.32,38 In 1955, Nutt43 reported the first good result in treating a patient with Brown's
syndrome using superior oblique tenectomy. However, it was not until 1976 that
a large study by Crawford38 showed the superiority of superior oblique tenotomy for correction of
this condition. In his retrospective review of 30 patients, one underwent
sheathotomy, nine underwent Z-tenotomy, two underwent split
tendon lengthening, 16 underwent complete tenotomy, and two were treated
with tenectomy. From this study, he concluded that tenotomy of the
superior oblique tendon gave the best results, with nine of 16 patients
obtaining normal or almost normal ocular movement. Eustis and associates,57 in a retrospective review of 30 patients, confirmed these relatively good
results, 26 of which had undergone either tenotomy or tenectomy. Again, division
of the superior oblique tendon nasal to the superior rectus
muscle was effective in eliminating the restriction of Brown's
syndrome. However, the authors also reported a high incidence of postoperative
decompensated superior oblique palsy. This condition was found
in 14 (54%) patients, and 10 (38%) required
further surgical treatment. These studies and others clearly show that complete tenotomy or tenectomy
of the superior oblique tendon is effective in reducing or eliminating
the motility disturbance and anomalous head posture in true Brown's
syndrome.32,62 However, careful attention to proper detail in surgical technique, especially
careful confirmation of the completeness of tenotomy with the
use of exaggerated force duction test, is necessary to maximize success
while minimizing the complication rate. Several studies have looked
at the short- and long-term results of silicone expander
for Brown's syndrome.59,60,62 Seawright and co-workers59 reported a subset of 13 patients with Brown's syndrome with preoperative
hypotropia in primary position who underwent the superior oblique
tendon expander procedure. The mean follow-up period for all
patients in the study was 28 months. Thirty-eight percent (five
patients) had complete resolution of vertical deviation if
primary gaze, and 54% (seven patients) had residual
but reduced vertical deviation in primary position (mean reduction
from 11 to four prism diopters). No patient manifested superior
oblique palsy at the last visit. Stager and co-workers60 reported similarly favorable results with their long-term study
on the silicone tendon expander. This retrospective study looked at 20 eyes
of 19 consecutive patients who underwent silicone expander procedure
for moderate to severe Brown's syndrome. A 6 to 10 mm expander
was placed in all patients. One hundred percent of patients had resolution
of their downshoot in adduction with some or full ability to
elevate the eye in adduction. The complication rate was relatively low
with 20% of patients requiring re-operation (consisting
of inferior oblique surgery) for significant overcorrection. One
patient extruded his silicone implant. Although there was a relatively
high incident of residual Brown's syndrome postoperatively (13 of 19 patients), all were converted from a severe to mild
Brown's syndrome, and the majority of these continued to improve
with time (up to 3 years postoperatively). Wright61 also has reported excellent short- (14/15, 93%) and
long-term (4/5, 80%) success using
the superior oblique silicone expander technique. No studies have looked at the long-term results of guarded tenotomy, or
compared them to the results of the silicone expander technique. Such
a study would be helpful, because its authors' opinion that
the guarded tenotomy may offer many of the advantages of the silicone
expander technique, without being as technically difficult, especially
in children, and without the added risk of implant extrusion. COMPLICATIONS AND THEIR MANAGEMENT As with other types of strabismus surgery, the most frequent adverse results
of the surgical treatment of true Brown's syndrome are under-corrections
or over-corrections. Under corrections, with
residual limitation of elevation in adduction, may be more common after
modified tendon-weakening procedures such as Z-tenotomy
of the tendon near its insertion, tenectomy of the posterior tendon
at its insertion, and superior oblique recession or split tendon-lengthening
procedures. However, under correction can also be seen
after superior oblique tenotomy or tenectomy, generally because of uncut
posterior tendon fibers that are missed at the time of surgery. This
complication can be minimized by careful attention to surgical detail, isolation
of the tendon under direct visualization, and especially, using
Guyton's exaggerated forced duction test to confirm that
a complete tenotomy has been performed. In addition, a patient sometimes
is seen who has an apparently complete tenotomy (documented by
exaggerated forced duction test) with an excellent initial result. Then, weeks
or months later, the patient develops a recurrence of
Brown's syndrome, presumably from reanastomosis or linking of the
severed tendon ends with fibrous scarring and then secondary scar contraction. Therefore, patients must be warned of possible late recurrence
of Brown's syndrome, even after an excellent initial surgical
result. Probably more common than under-correction is early or delayed over-correction, with development of a decompensated superior oblique
palsy, head tilt, and inferior oblique overaction. The incidence
of this complication has ranged from 20% to 85% in recent
studies.32,57,59,63 In these studies, 20% to 82% of patients required additional
surgery for treatment of iatrogenic superior oblique palsy.32,57 To reduce the incidence of superior oblique palsy and the need for secondary
surgery, some surgeons combine an inferior oblique weakening procedure
with the superior oblique tenotomy for Brown's syndrome. Parks
and Eustis58 reported the results of combining 14-mm recession of the inferior
oblique with tenotomy of the superior oblique in 16 eyes of patients
with Brown's syndrome. Good or excellent results were obtained
in 94% of eyes, and further surgery was not needed. However, inferior
oblique under action, with many features similar to under-correction
of Brown's syndrome, was seen in 75% of eyes
immediately after surgery. Although this elevation deficit in adduction
improved over time, Parks and Eustis58 recommended reducing the amount of inferior oblique recession from 14 to 10 mm. Alternatively, a controlled tenotomy, such as the superior oblique silicone
tendon expander operation, may yield as good an initial surgical
result without later overcorrection.57,60 Further controlled studies are needed to show superiority of this technique
over the simpler tenotomy, with or without simultaneous inferior
oblique weakening. Care must be taken to monitor the binocular status of all patients before
and after surgery for Brown's syndrome.64, 65 Although Sprunger co-worker64 reported improvement in binocular vision with superior oblique weakening
of various types, Eustis and colleagues65 reported a loss of binocularity in 11% of 17 patients who underwent
tendon surgery for Brown's syndrome. Altered alignment after
surgery, especially in very young patients, may result in suppression
with eventual loss of binocularity. Postponing correction in young infants
with evidence of fusion may reduce this risk. With respect to complications associated with the silicone expander, Wilson
and co-workers66 reported two cases of late down gaze restriction following the silicone
tendon expander procedure, both which were secondary to adhesions between
the superior oblique tendon and nasal border of the superior rectus
muscle. Stager and co-workers60 did not observe this complication in any of their cases, and advised the
use of a narrower #40 silicone implant (rather than the #240) as
well as careful attention to preservation of the inner
layer of the intermuscular septum, as means of avoiding this problem. Many other complications that have been reported in patients treated surgically
for Brown's syndrome are related to poor surgical judgment
or technique. Tendon isolation for superior oblique tenotomy by blindly
sweeping 10 to 12 mm posteriorly through a superonasal fornix incision, as
described by Berke,41 has been associated with paresis or inadvertent transection of the superior
rectus,45,49 permanent blepharoptosis, massive hemorrhage from rupture of a vortex
vein, and rupture of Tenon's capsule with resultant prolapse of orbital
fat and possible development of fat adherence syndrome. These complications
should be eliminated by isolation of the superior oblique
tendon by direct visualization, as described by Parks and Helveston.46,47 With careful attention to surgical anatomy and technique, as described, superior
oblique tenotomy, with or without inferior oblique recession, can
safely and effectively eliminate the clinically significant motility
disorder in Brown's syndrome, with minimal complications. |