SKIN
The upper eyelid skin is the thinnest in the body, with the lower eyelid skin being only slightly thicker. There is very minimal dermal tissue associated with eyelid skin; therefore, less substantial scarring occurs in this area when compared with the periorbital tissues. The periorbital, forehead, and cheek skin is considerably thicker, with a much more substantial dermal layer. The upper eyelid skin merges into the thicker forehead and glabellar skin at the superior orbital rim and eyebrow.
The major anatomic features of the upper eyelids include the eyelid crease and fold and the eyelashes. The normal crease is approximately 10 mm superior to the upper eyelid margin.5–8 There is some variation to this, with the eyelid crease in Asians being considerably lower in many individuals.1 The upper eyelid crease represents the point at which slips of the levator muscle interdigitate with the orbicularis muscle to insert into the undersurface of the skin. Recession of the eyelid crease associated with traumatic ptosis suggests an underlying dehiscence of the levator aponeurosis. A change in the eyelid crease can also occur after eyelid surgery or laceration repair where the aponeurotic interdigitations are disrupted.
The eyelid fold represents the point at which the looser preseptal skin overhangs the more firmly attached pretarsal skin when the eyelid is open. The full appearance of the preseptal area of the eyelid is due to the underlying fat. In Asians there is a lower eyelid fold due to both the lower attachments of the levator muscle and the lower attachment of the septum onto the levator allowing the anterior and inferior extent of the orbital fat to be at a lower level on the tarsus.1 Loss of upper eyelid fullness can be associated with orbital fractures or post-traumatic or inflammatory fat necrosis.9,10
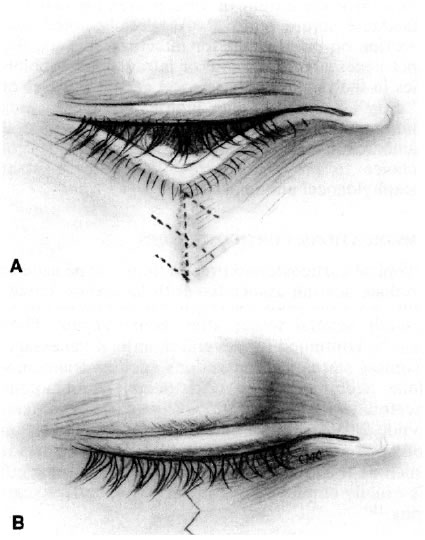
The features of the lower eyelid are less distinct than the upper. Although there is a lower eyelid crease in most individuals it is not as distinct as that in the upper eyelid. However, the pretarsal skin is more firmly attached than the preseptal skin, and a crease may be seen 2 to 4 mm below the eyelid margin, especially in downgaze. Other creases occur in the lower eyelid and in the lateral temporal periorbital skin as aging occurs. Like the upper eyelid, the preseptal fullness to the lower eyelid is due to the presence of orbital fat. An asymmetric reduction in this fullness can be associated with orbital fractures and fat necrosis. The lower eyelid skin merges into the thick skin of the cheek at the inferior orbital rim. A malar fat pad can be found beneath the thick skin and muscle over the zygomatic bone as it forms the lateral aspect of the inferior orbital rim.
ORBICULARIS MUSCLE, MEDIAL CANTHAL TENDON, AND LATERAL CANTHAL TENDON
The next layer below the eyelid skin and dermis is the orbicularis muscle. This muscle is shaped like a sphincter with attachments medially forming the medial canthal tendon and laterally forming the lateral canthal raphe. The muscle extends to the eyelid margin where it forms the muscle of Riolan, which is seen as the gray line just anterior to the openings of the meibomian glands. Superiorly the muscle extends under the eyebrow. The facial nerve provides the innervation to this structure and can be damaged with large lacerations involving the lateral face.
Laterally, the fibers of the orbicularis muscle from the upper and lower eyelids interdigitate or become a raphe. A small tendon extends from this raphe and inserts onto the lateral orbital tubercle, which is located several millimeters inside the orbital rim. A small fat pad can be found in some individuals beneath this tendon.2 It is important to resuture the eyelids inside the orbital rim when repairing lateral canthal lacerations to prevent gaping between the eyelids and the globe.
The medial canthal ligament has two heads, a superficial head that inserts onto the anterior lacrimal crest and a deep one that inserts onto the posterior lacrimal crest.11 These two tendons surround the lacrimal sac, which sits in the lacrimal fossa. The deep or posterior limb of the tendon is formed by the deep heads of the pretarsal and preseptal portions of the orbicularis muscle. The anterior limb of the tendon is formed by the superficial heads of the preseptal and pretarsal orbicularis muscle. There is also a superior supporting branch of the anterior limb that inserts onto the frontal bone.11 The integrity of this structure and of the deep head of the tendon are important for preventing post-traumatic medial canthal dystopia. The upper and lower canaliculi and common canaliculus are directly below the superficial limb of the medial canthal tendon. These structures should be considered involved in all medial canthal injuries until probing and irrigation of the lacrimal system has been performed.
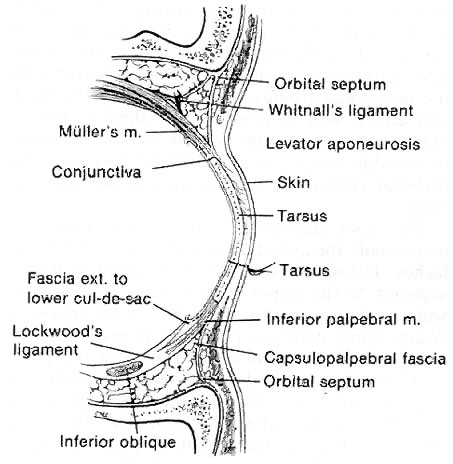
ORBITAL SEPTUM AND FAT
The orbital septum is an extension of the orbital rim periosteum. Superiorly this structure inserts onto the levator aponeurosis several millimeters above the level of the superior tarsal border. As already noted this can vary from individual to individual, with a much lower attachment being present in most Asians. In the lower eyelid the orbital septum attaches to the lower eyelid retractors approximately at the level of the inferior tarsal border. Behind the septum in the upper eyelid are two fat pads, one medially placed and one centrally placed. Laterally, the orbital portion of the lacrimal gland is present behind the septum. The fat pads are just anterior to the levator muscle and aponeurosis. In the lower eyelid there are three fat pads: medial, central, and lateral. They lie just anterior to the capsulopalpebral fascia, which is the analogue of the levator in the upper eyelid.
EYELID RETRACTORS
In the upper eyelid the eyelid retractors are Müller's (or the superior tarsal) muscle and the levator aponeurosis and muscle. In the lower eyelid they are the capsulopalpebral fascia and Müller's (or the inferior tarsal) muscle. The levator muscle originates just above the superior rectus muscle in the posterior orbit traveling anteriorly before changing direction at Whitnall's ligament and becoming an aponeurosis that ultimately inserts onto the anterior surface of the tarsus. Like the superior rectus muscle the superior division of the oculomotor nerve innervates the levator muscle. At Whitnall's ligament the aponeurosis fans out to form the so-called horns. The lateral horn separates the lacrimal gland into palpebral and orbital portions. Whitnall's ligament and the lateral horn of the aponeurosis attach onto the lateral orbital tubercle and contribute to the lateral canthal tendon. The aponeurosis lies behind the orbital septum and fat. It is only loosely connected to the orbicularis muscle anteriorly except for the slips of tissue that form the eyelid crease. This potential space between the aponeurosis and the orbicularis muscle is utilized in the anterior surgical approach to the eyelid as a way of avoiding damage to the aponeurosis. Identification of the orbital septum and fat is an important landmark during aponeurosis surgery or laceration repair.
Müller's muscle is a sympathetically innervated muscle immediately posterior to the levator aponeurosis. It is only loosely attached to the aponeurosis and can be easily dissected from it. Müller's muscle is 10 to 12 mm in height. It inserts onto the superior tarsal border and originates from the levator muscle. Posteriorly, conjunctiva is only minimally adherent to it. The peripheral palpebral arterial arcade travels on the anterior surface of Müller's muscle just superior to its insertion into the tarsus. This is an important landmark for identifying the muscle.
In the lower eyelid the capsulopalpebral fascia and inferior tarsal border are usually considered as one structure. Anteriorly there is a potential space between the orbicularis muscle and the eyelid retractors that can be utilized during lower eyelid surgery as an avascular plane for dissection. Posteriorly, the conjunctiva can be relatively easily dissected from this structure. Dehiscence of the lower eyelid retractors from the tarsus is thought in some cases to be associated with involutional entropion. Scarring between the septum and the retractors commonly occurs after orbital fracture repair, resulting in lower eyelid retraction.
TARSUS
The tarsus is a dense connective tissue structure that forms the basic support for the eyelid. There are about 25 meibomian glands contained in the upper eyelid tarsus and 20 in the lower. The tarsus is 1 mm thick and 26 to 28 mm long. The height of the upper eyelid tarsus is about 10 mm and that of the lower eyelid is 3.5 to 5 mm.12 Müller's muscle is attached to the superior tarsal border of the upper eyelid and the inferior tarsal border of the lower eyelid. The tarsus ends at the eyelid margin. The levator aponeurosis attaches to the inferior two thirds of the anterior surface of the tarsus. There is a potential space between the superior one third of the tarsus and the aponeurosis. The capsulopalpebral fascia inserts onto the anterior surface of the lower eyelid tarsus and Müller's muscle onto the inferior border of this structure. In both the upper and lower eyelids the marginal artery travels between the orbicularis muscle and the tarsus 3 to 4 mm from the eyelid margin.
CONJUNCTIVA
The conjunctiva lines the posterior surface of the eyelids reflecting upon itself at the superior and inferior fornices to become the bulbar conjunctiva covering the globe. The palpebral conjunctiva is firmly attached at the eyelid margin and to the tarsus. It is less firmly attached to Müller's muscle and can be fairly easily dissected from this structure or ballooned away from it with saline. There is some redundancy to the conjunctiva, and a portion of it can be excised or lost without compromising either eyelid or globe function or reducing the goblet cell contribution to the tear film. In the lateral aspect of the upper eyelid and superior fornix is the palpebral lobe of the lacrimal gland and the lacrimal ductules. Deep lacerations of the eyelid can damage these structures, reducing the aqueous portion of the tear film.
EYELID MARGIN
The eyelid margin represents a sandwich of tissues. Its most posterior layer is the nonkeratinized epithelium of the conjunctiva. This becomes keratinized at the mucocutaneous junction at the posterior border of the tarsus. The tarsus is the next most anterior layer and contains the orifices of the meibomian glands. The gray line or muscle of Riolan, which represents the edge of the orbicularis muscle is just anterior to the tarsus.13 The eyelid skin and eyelashes comprise the most anterior layer. Eyelashes are more numerous in the upper eyelid, which may contain two to four irregular rows of cilia. The lower eyelid contains one or two rows of eyelashes. The most medial aspect of the upper and lower eyelid margin contains a lacrimal punctum. Each is approximately 5 mm from the medial canthal angle. The puncta are nipple-like openings surrounded by a muscular sphincter. They are usually slightly inturned toward the tear lake. The tarsus ends at the punctal opening. Though not part of the eyelid margin, the caruncle, a nodular continuation of the conjunctiva containing both glandular tissue and cilia is just posterior to the medial termination of the eyelids at the medial canthal angle.
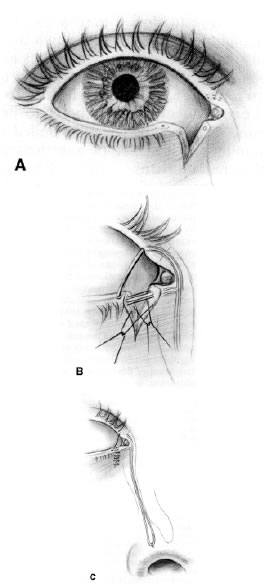
The puncta and vertical portion of the canaliculi are 1 to 2 mm long, becoming horizontal at a dilatation called the ampulla. The horizontal portion of the canaliculi is about 8 mm long, becoming one structure at the common canaliculus, which is 1 to 3 mm in length.14 The puncta are 0.3 mm in diameter while the canaliculi are 1 to 2 mm in diameter.14 Although initially traveling in the superficial and posterior aspect of the medial eyelid, the canaliculi dive deep into the eyelid and medial canthal tissue until they are below the superficial limb of the medial canthal tendon. The common canaliculus enters the lacrimal sac at the junction of its superior one third and inferior two thirds. The lacrimal sac is 15 mm in height, with 3 to 5 mm of it above the medial canthal tendon and the rest below the tendon.14 The lacrimal sac becomes the nasolacrimal duct in the bony nasolacrimal canal at the inferior orbital rim as it merges with the anterior lacrimal crest. The nasolacrimal duct enters the nose in the inferior meatus approximately 4 cm posterior to the opening of the nares. The canaliculi are lined with nonkeratinized stratified squamous epithelium. When cut, they have a grayish appearance. The lacrimal sac and duct are lined with modified, nonciliated respiratory epithelium.
EYEBROWS
The upper eyelid skin merges into the thicker skin of the eyebrow and forehead area at the superior orbital rim. The inferior aspect of the male eyebrow begins at the superior orbital rim. The female eyebrow is usually at a slightly higher level. The eyebrow is widest medially where it overlies the frontal sinus and is narrowest laterally. It forms a mild arch as it extends over the superior orbital rim. The eyebrows are separated by the skin of the glabellar area just above the nasal root. There is a thick layer of muscle beneath the eyebrows. Under this is the eyebrow fat pad and the deep insertion of the galea aponeurotica.
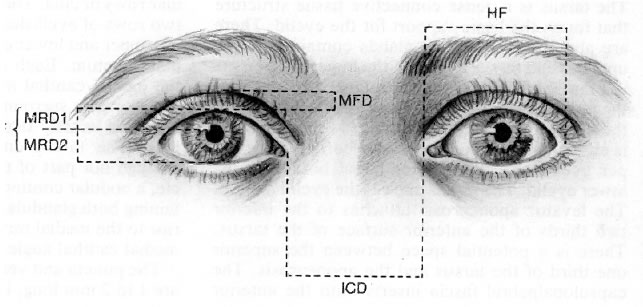
NORMAL MEASUREMENTS
The normal palpebral fissure is 26 to 30 mm in horizontal dimension and 8 to 10 mm in height (Fig. 2).7,8,15 The distance from the pupillary light reflex to the upper eyelid (MRD-1) ranges between 2.5 and 5.0 mm and the distance from pupillary light reflex and the lower eyelid (MRD-2) is between 4.5 and 5.5 mm.7,8 The normal upper eyelid rests 1 to 2 mm below the 12 o'clock border of the limbus, and the lower eyelid rests just at the 6 o'clock border of the limbus, although it may also be slightly above or below this level.16,17 The distance between the two medial canthi is normally 30 to 34 mm.15 In young individuals, 6 to 8 mm of full-thickness eyelid and margin may be removed and the defect repaired primarily. In older individuals it may be possible to remove as much as 12 to 14 mm of eyelid and still achieve primary closure. The puncta are approximately 6 to 7 mm from the medial canthal angle. The medial canthal angle is 0 to 2 mm below the level of the lateral canthal angle in most individuals.15 The tarsus is approximately 1 mm in thickness and 24 to 28 mm in length.1 The height of the upper eyelid tarsus is usually 10 mm, and the average height of the lower eyelid tarsus is 3.7 mm.1,12