1. Bell JA: Eye trauma in sports: a preventable epidemic. JAMA 246:156, 1981 2. Parver LM: Eye trauma. The neglected disorder. Arch Ophthalmol 104:1452, 1986 3. Vinger PF: Sports eye injuries a preventable disease. Ophthalmology 88:108, 1981 4. Pashby T: Personal communication; 1994. 5. Rivara FP, Grossman DC, Cummings P: Injury prevention. Second of two parts. N Engl J Med. 337:613, 1997 6. Rivara FP, Grossman DC, Cummings P: Injury prevention. First of two parts. N Engl J Med. 337:543, 1997 7. Vinger PF: Injury prevention: where do we go from here? J Am Optom Assoc 70:87, 1999 8. Viano DC: A blueprint for injury control in the United States. Public Health Rep 105:329, 1990 9. Clarke KS: Premises and pitfalls of athletic injury surveillance. J Sports Med 3:292, 1975 10. National Institutes of Health.:Conference on Sports Injuries in Youth: Surveillance
Strategies; April 8–9, 1991; Bethesda, MD 11. Doege TC: Sounding board. An injury is no accident. N Engl J Med 298:509, 1978 12. Doege TC, Gelfand HM: A model for epidemiologic research. JAMA 239:328, 1978 13. Dalma-Weiszhausz J: Extrabulbar tissue prolapse. In Kuhn F, Poeramici DJ, eds. Ocular Trauma: Principles and Practice. New York: Thieme, 2002:123–130 14. Danis RP, Neely D, Plager DA: Unique aspects of trauma in children. In Kuhn F, Pieramici DJ, eds. Ocular Trauma: Principles and Practice. New York: Thieme, 2002:307–319 15. Apte RS, Scheufele TA, Blomquist PH: Etiology of blindness in an urban community hospital setting. Ophthalmology 108:693, 2001 16. Vinger PF: The incidence of eye injuries in sports. In Vinger PF, ed. Ocular Sports Injuries. Vol. 21. Boston: Little, Brown and Company, 1981:21–46. 17. Karlson TA, Klein BE: The incidence of acute hospital-treated eye injuries. Arch Ophthalmol 104:1473, 1986 18. Rapoport I, Romem M, Kinek M, et al: Eye injuries in children in Israel. A nationwide collaborative study. Arch Ophthalmol 108:376, 1990 19. Schein OD, Hibberd PL, Shingleton BJ, et al: The spectrum and burden of ocular injury. Ophthalmology 95:300, 1988 20. Jones NP: Eye injury in sport. Sports Med 7:163, 1989 21. Jones NP: One year of severe eye injuries in sport. Eye 2(Pt 5):484, 1988 22. Grin TR, Nelson LB, Jeffers JB: Eye injuries in childhood. Pediatrics 80:13, 1987 23. Erie JC, Nevitt MP, Hodge D, et al: Incidence of enucleation in a defined population. Am J Ophthalmol 113:138, 1992 24. Sheps SB, Evans GD: Epidemiology of school injuries: a 2-year experience in a municipal
health department. Pediatrics 79:69, 1987 25. Strahlman E, Elman M, Daub E, et al: Causes of pediatric eye injuries. A population-based study. Arch Ophthalmol 108:603, 1990 26. Lavrich J, Goldberg D, Nelson L, et al: Visual outcome of severe eye injuries during the amblyogenic years. Binocular Vision 9:3, 1994 27. Gregory PT: Sussex Eye Hospital sports injuries. Br J Ophthalmol 70:748, 1986 28. Larrison WI, Hersh PS, Kunzweiler T, et al: Sports-related ocular trauma. Ophthalmology 97:1265, 1990 29. Jaison SG, Silas SE, Daniel R, et al: A review of childhood admission with perforating ocular injuries in a hospital
in north-west India. Indian J Ophthalmol 42:199, 1994 30. Gallagher SS, Finison K, Guyer B, et al: The incidence of injuries among 87,000 Massachusetts children and adolescents: results
of the 1980–81 Statewide Childhood Injury Prevention
Program Surveillance System. Am J Public Health 74:1340, 1984 31. Powell JW: Pros and cons of data-gathering mechanisms. In Vinger P, Hoerner E, eds. Sports Injuries: The Unthwarted Epidemic. 2nd ed. Littleton, MA: PSG Publishing Company, Inc., 1986:28–32 32. NEISS. Washington, DC: National Electronic Injury Surveillance System. US Consumer Product Safety Commission/Directorate for Epidemiology, National
Injury Information Clearinghouse; 1984–2001 33. Parver LM, Dannenberg AL, Blacklow B, et al: Characteristics and causes of penetrating eye injuries reported to the
National Eye Trauma System Registry, 1985–91. Public Health Rep 108:625, 1993 34. Vinger PF: The need for standardization for protective eyewear in sports. In Kuhn F, Poeramici DJ, eds. Ocular Trauma: Principles and Practice. New York: Thieme, 2002:455–460 35. SGMA International. Sports Participation in America. 2002:21, North Palm Beach, FL. 36. Strahlman E, Sommer A: The epidemiology of sports-related ocular trauma. Int Ophthalmol Clin 28:199, 1988 37. Dick R, ed: NCAA Health and Safety Injury Surveillance System. Indianapolis, IN NCAA; 1989–2002 38. Tielsch JM, Parver LM: Determinants of hospital charges and length of stay for ocular rauma. Ophthalmology 97:231, 1990 39. Prunella W: Injury Cost model. 1999. Located at: Average societal cost of body part injured, Bethesda, MD 40. Feist RM, Farber MD: Ocular trauma epidemiology. Arch Ophthalmol 107:503, 1989 41. Tolpin HG, Vinger PF, Tolpin DW: Ocular sports injuries. Economic considerations. Int Ophthalmol Clin 21:179, 1981 42. Breslow L, Somers AR: The lifetime health-monitoring program. A practical approach to
preventive medicine. N Engl J Med 296:601, 1977 43. Bloomfield L: How Things Work: The Physis of Everyday Life. New York: John Wiley & Sons, Inc., 1997. 44. Berger R: A model for evaluating the ocular contusion injury potential of propelled
objects. J Bioeng 2:345, 1987 45. Preston J: Review of standard consumer safety specification for non-powder
guns (ANSI/ASTM F589–78) and non-powder gun projectiles
and propellants (ANSI/ASTM F590–78). Washington, DC: Mechanical and Textile Division, Engineering Sciences, CPSC, 1980 46. Delori F, Pomerantzeff O, Cox MS: Deformation of the globe under high-speed impact: it relation to
contusion injuries. Invest Ophthalmol 8:290, 1969 47. Berger R: Impact on human eyes by propelled objects. 1980. In Report to Consumer Product Safety Commission NBSIR 80–2037, Bethesda, MD. 48. Berger R: System for assessing eye injury potential of propelled objects. J Res Natl Bureau Standards 84:9, 1979 49. Stitzel JD, Duma S, Cormier J, et al: A nonlinear finite element model of the eye with experimental validation
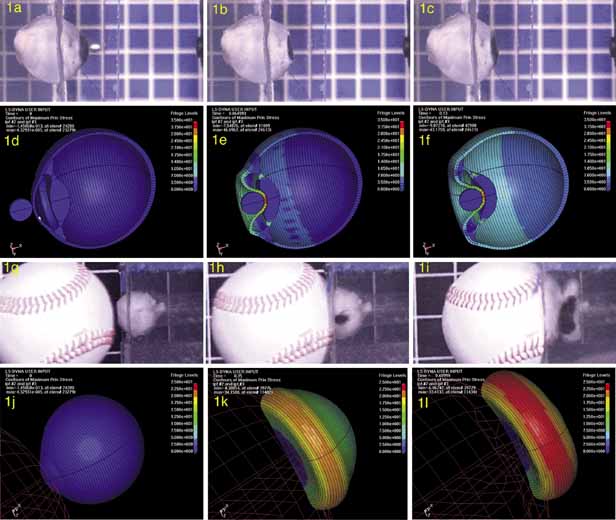
for the prediction of globe rupture. Stapp Car Crash J 46:81, 2002 50. Power ED, Duma SM, Stitzel JD, et al: Computer modeling of airbag-induced ocular injury in pilots wearing
night vision goggles. Aviat Space Environ Med 73:1000, 2002 51. Uchio E, Ohno S, Kudoh J, et al: Simulation model of an eyeball based on finite element analysis on a supercomputer. Br J Ophthalmol 83:1106, 1999 52. Uchio E, Ohno S, Kudoh K, et al: Simulation of air-bag impact on post-radial keratotomy eye
using finite element analysis. J Cataract Refract Surg 27:1847, 2001 53. Crocker J, DesRochers C, Delbridge G, et al: Optimization of lens edge design for safety eyewear using experimentally
validated finite element (FE) impact analysis. Paper presented at: 7th International Conference on Product Safety Research, 1999; Bethesda, MD 54. Kuhn F, Morris R, Witherspoon CD, et al: A standardized classification of ocular trauma. Graefes Arch Clin Exp Ophthalmol 234:399, 1996 55. Duke-Elder S, MacFaul P: Injuries: Part 1. Mechanical Injuries. Vol. 14. St. Louis: C.V. Mosby Company, 1972 56. Jonas JB, Mardin CY, Schlotzer-Schrehardt U, et al: Morphometry of the human lamina cribrosa surface. Invest Ophthalmol Vis Sci 32:401, 1991 57. Olsen TW, Aaberg SY, Geroski DH, et al: Human sclera: thickness and surface area. Am J Ophthalmol 125:237, 1998 58. Funata M, Tokoro T: Scleral change in experimentally myopic monkeys. Graefes Arch Clin Exp Ophthalmol 228:174, 1990 59. Friberg TR, Lace JW: A comparison of the elastic properties of human choroid and sclera. Exp Eye Res 47:429, 1988 60. Jandeck C, Kellner U, Bornfeld N, et al: Open globe injuries in children. Graefes Arch Clin Exp Ophthalmol 238:420, 2000 61. Hahn HJ: Perforating wounds of the eye. J R Nav Med Serv 62:73, 1976 62. Kuhn F, Maisiak R, Mann L, et al: The OTS: Predicting the final vision in the injured eye. In Kuhn F, Pieramici DJ, eds. Ocular Trauma: Principles and Practice. New York: Thieme, 2002:9–13 63. Pieramici DJ, MacCumber MW, Humayun MU, et al: Open-globe injury. Update on types of injuries and visual results. Ophthalmology 103:1798, 1996 64. Esmaeli B, Elner SG, Schork MA, et al: Visual outcome and ocular survival after penetrating trauma. A clinicopathologic
study. Ophthalmology 102:393, 1995 65. Eide N, Syrdalen P: Contusion rupture of the globe. Acta Ophthalmol Suppl 182:169, 1987 66. Vinger PF, Duma SM, Crandall J: Baseball hardness as a risk factor for eye injuries. Arch Ophthalmol 117:354, 1999 67. Vinger PF: Injury to the postsurgical eye. In Kuhn F, Pieramici DJ, eds. Ocular Trauma: Principles and Practice. New York: Thieme, 2002:280–292 68. Peacock LW, Slade SG, Martiz J, et al: Ocular integrity after refractive procedures. Ophthalmology 104:1079, 1997 69. Potts AM, Distler JA: Shape factor in the penetration of intraocular foreign bodies. Am J Ophthalmol 100:183, 1985 70. Offutt RL, Shine I: Perforating injuries of the eye due to glass. Ann Ophthalmol 6:357, 1974 71. Keeney A, Estlow B: Spectacle glass injuries to the eye. Am J Ophthalmol 72:12, 1971 72. Keeney A, Renaldo D: Newly defined lens and frame factors in the reduction of eye injuries. Eye Ear Nose Throat Monthly 52:48, 1973 73. Keeney AH: Estimating the incidence of spectacle lens injuries. Am J Ophthalmol 73:289, 1972 74. Christianson MD, Parker JA, Arndt J: Material and thickness: the important factors in the impact resistance
of spectacle lenses. Can J Ophthalmol 12:300, 1977 75. Easterbrook M: Eye injury: assessment and prevention in sports. Mod Med Can 46:14, 1991 76. Easterbrook M: Eye protection in the racket sports: An update. Phys Sportsmed 15:180, 1987 77. Keeney AH, Fintelmann E, Renaldo D: Clinical mechanisms in non-industrial spectacle trauma. Am J Ophthalmol 74:662, 1972 78. Dannenberg AL, Parver LM, Brechner RJ, et al: Penetration eye injuries in the workplace. The National Eye Trauma System
Registry. Arch Ophthalmol 110:843, 1992 79. Orlando RG: Soccer safety. Phys Sportsmed 19:62, 1991 80. Barker-Griffith AE, Streeten BW, Abraham JL, et al: Potato gun ocular injury. Ophthalmology 105:535, 1998 81. Keeney AH, Fintelmann E, Estlow B: Refractive correction and associated factors in spectacle glass injury. Arch Ophthalmol 88:2, 1972 82. Safe spectacles and sunglasses for all. JAMA 213:2071, 1970 83. Schepens CL: Pathogenesis of Traumatic Retinal Detachment. In Freeman H, ed. Ocular Trauma. New York: Appelton-Century-Crofts, 1979:273–284 84. Kroll P, Stoll W, Kirchhoff E: [Contusion-suction trauma after globe injuries]. Klin Monatsbl Augenheilkd 182:555, 1983 85. Campbell DG: Traumatic glaucoma. In Shingleton BJ, Hersh PS, Kenyon KR, eds. Eye Trauma. St. Louis: Mosby-Year Book, Inc., 1991:117–125 86. Thompson JT: Traumatic retinal tears and detachents. In Shingleton BJ, Hersh PS, Kenyon KR, eds. Eye Trauma. St. Louis: Mosby-Year Book, Inc., 1991:195–203 87. Bressler S, Bressler N: Traumatic maculopathies. In Kenyon KR, ed. Eye Trauma. St. Louis: Mosby-Year Book, Inc., 1991:187–194 88. Cox MS, Schepens CL, Freeman HM: Retinal detachment due to ocular contusion. Arch Ophthalmol 76:678, 1966 89. Ikeda N, Ikeda T, Nagata M, et al: Pathogenesis of transient high myopia after blunt eye trauma. Ophthalmology 109:501, 2002 90. Beiran I, Miller B: Pure ocular blast injury. Am J Ophthalmol 114:504, 1992 91. Leibsohn J, Burton TC, Scott WE: Oribital floor fractures: a retrospective study. Ann Ophthalmol 8:1057, 1976 92. Keeney AH: Discussion of: Vinger PF: Sports eye injuries: A preventable disease. Ophthalmology 88:108, 1981 93. Iskander NG, Peters NT, Anderson Penno E, et al: Late traumatic flap dislocation after laser in situ keratomileusis. J Cataract Refract Surg 27:1111, 2001 94. Lombardo AJ, Katz HR: Late partial dislocation of a laser in situ keratomileusis flap. J Cataract Refract Surg 27:1108, 2001 95. Melki SA, Talamo JH, Demetriades AM, et al: Late traumatic dislocation of laser in situ keratomileusis corneal flaps. Ophthalmology 107:2136, 2000 96. Patel CK, Hanson R, McDonald B, et al: Case reports and small case series: late dislocation of a LASIK flap caused
by a fingernail. Arch Ophthalmol 119:447, 2001 97. Schwartz GS, Park DH, Schloff S, et al: Traumatic flap displacement and subsequent diffuse lamellar keratitis after
laser in situ keratomileusis. J Cataract Refract Surg 27:781, 2001 98. Dudenhoefer EJ, Vinger PF, Azar DT: Trauma after refractive surgery. Int Ophthalmol Clin 42:33, 2002 99. Aldave AJ, Hollander DA, Abbott RL: Late-onset traumatic flap dislocation and diffuse lamellar inflammation
after laser in situ keratomileusis. Cornea. 21:604, 2002 100. Geggel HS, Coday MP: Late-onset traumatic laser in situ keratomileusis (LASIK) flap
dehiscence. Am J Ophthalmol 131:505, 2001 101. Fulmek R: [Chiasma lesions in sport accidents (author's transl)]. Klin Monatsbl Augenheilkd 167:445, 1975 102. Chow AY, Goldberg MF, Frenkel M: Evulsion of the optic nerve in association with basketball injuries. Ann Ophthalmol 16:35, 1984 103. Deodati F, Bec P, Peyresblanques J, et al: [Oculo-orbital injuries of skiers]. Ann Ocul (Paris) 202:953, 1969 104. Dutton GN, Heron G, Diaper C: Baseball hitting and the Pulfrich phenomenon: could it be due to traumatic
optic neuropathy? Arch Ophthalmol 115:1344, 1997 105. Fard AK, Merbs SL, Pieramici DJ: Optic nerve avulsion from a diving injury. Am J Ophthalmol 124:562, 1997 106. Friedman SM: Optic nerve avulsion secondary to a basketball injury. Ophthalmic Surg Lasers 30:676, 1999 107. Killer HE, Blumer BK, Rust ON: Avulsion of the optic disc after a blow to swimming goggles. J Pediatr Ophthalmol Strabismus 36:92, 1999 108. Roth DB, Warman R: Optic nerve avulsion from a golfing injury. Am J Ophthalmol 128:657, 1999 109. Weinberger DG, Selesnick SH: Roller blade falls—a new cause of temporal bone fractures: case reports. J Trauma 3:500, 1974 110. Oh S, Ruedi M: Depressed skull fracture in skiing and its experimental study. Int J Sports Med 3:169, 1982 111. Kelly KD, Lissel HL, Rowe BH, et al: Sport and recreation-related head injuries treated in the emergency
department. Clin J Sport Med 11:77, 2001 112. O'Rourke NA, Costello F, Yelland JD, et al: Head injuries to children riding bicycles. Med J Aust 146:619, 1987 113. Bishop PJ: Head protection in sport with particular application to ice hockey. Ergonomics 19:451, 1976 114. Saczalski KJ, Richardson EQ: Nonlinear numerical prediction of human head/helmet crash impact response. Aviat Space Environ Med 49(1 Pt. 2):114, 1987 115. Benson BW, Mohtadi NG, Rose MS, et al: Head and neck injuries among ice hockey players wearing full face shields
vs half face shields. JAMA 282:2328, 1999 116. Vinger P, Easterbrook M, Hirschfelder D: Sports eye injuries. A model for prevention. JAMA 250:3322, 1983 117. Duke-Elder S, Wybar K: The Anatomy of the Visual System. Vol 2. St. Louis: C.V. Mosby Company, 1961 118. Hotte H: Orbital Fractures. Springfield, IL: Charles C Thomas, 1970. 119. Swearington J: Tolerances of the human face to crash impact. Oklahoma City: Federal Aviation Agency, 1965 120. Bishop P: Ice hockey helmets: using a mathematical model of head protection for evaluating
standards. J Safety Res 8:163, 1976 121. Hughes J, Wilms J, Adams C: Football helmet evaluation based on players EEG's. Phys Sportsmed 5:73, 1977 122. Whalley J: When can standards create antitrust problems? ASTM Standardization News p. 46, January 1990 123. Burke MJ, Sanitato JJ, Vinger PF, et al: Soccerball-induced eye injuries. JAMA 249:2682, 1983 124. Halstead P: Performance testing updates in head, face and eye protection. J Athletic Training 36:322, 2001 125. Pashby T: Standards reduce eye injuries in sports. In Henkind P, ed. Acta: XXIV International Congress of Ophthalmology. Philadelphia: JB Lippincot, 1983, pp. 1053–1055 126. Vinger P: Eye safety testing and standards. Ophthalmol Clin North Am 12:345, 1999 127. Hulse W: Sports equipment standards. In Vinger P, Hoerner E, eds. Sports Injuries: The Unthwarted Epidemic. Littleton, MA: Publishing Sciences Group, 1981:378–382 128. Milner E: Sports safety standards and sports safety. ASTM Stand News pp. 1–11, June 1992 129. Canadian Standards Association: Racket Sports Eye Protection, Preliminary
Standard. Toronto: Canadian Standards Association, 1986 130. Exploding golf balls. Bull Natl Clgh Poison Control Cent July-Aug:2, 1971 131. Bishop P: A comparison of selected headforms under impact conditions. Report to the Canadian Standards Association technical committee on protective
equipment for hockey and lacrosse players. 1988 132. Hodgson V: Impact standards for protective equipment. In Torg J, ed. Athletic Injuries to the Head, Neck, and Face. St. Louis: CV Mosby, 1991:28–43 133. Farkas L, Munro I: Anthropometric Facial Proportions in Medicine. Springfield, IL: Charles C. Thomas, 1987, pp. 378–381 134. Morehouse C: Obsolescence in protective equipment. In Vinger P, Hoerner E, eds. Sports Injuries: The Unthwarted Epidemic. Littleton, MA: Publishing Sciences Group, 1981 135. American Academy of Pediatrics Committee on Sports Medicine: Recommendations
for participation in competitive sports. Pediatrics 81:737, 1988 136. Moeller J: Contraindications to athletic participation: spinal systemic, dermatologic, paired-organ, and other issues. Phys Sportsmed 24:57, 1996 137. Moeller J: Contraindications to athletic participation: cardiac, respiratory, and
central nervous system conditions. Phys Sportsmed 24:47, 1996 138. Medical Evaluation of the Athlete: A Guide: Chicago: American Medical Association, 1976. 139. Dyment P: New guidelines for sports participation. Phys Sportsmed 16:45, 1988 140. Mitten M: When is disqualification from sports justified? Medical judgment
vs patient's rights. Phys Sportsmed 24:75, 1996 141. Knuttgen HG: Eye injuries and eye protection in sports: a position statement from the
International Federation of Sports Medicine. Int J Sports Med 9:474, 1988 142. Steiner GC, Peterson LW: Severe emotional response to eye trauma in a child: awareness and intervention. Arch Ophthalmol 110:753, 1992 143. Singular Vision Outreach. PO Box 1451, Maryland Heights, MO 63043 144. Kaplan PJ: Ocular sports injuries. Legal aspects. I. Patient's perspective. Int Ophthalmol Clin 21:203, 1981 145. Tommila V, Tarkkanen A: Incidence of loss of vision in the healthy eye in amblyopia. Br J Ophthalmol 65:575, 1981 146. Vinger P: Preventing ocular injuries. Am Orthoptic J 32:56, 1982 147. Vinger P: The one-eyed athlete. Phys Sportsmed 15:48, 1987 148. Dorsen P: Should athletes with one eye, kidney, or testicle play contact sports? Phys Sportsmed 14:130, 1986 149. American Academy of Pediatrics: American Academy of Pediatrics Policy Statement: Recommendations
for participation in competitive sports. Phys Sportsmed 16:165, 1988 150. Magnes S, Henderson J, Hunter S: What conditions limit sports participation? Phys Sportsmed 20:143, 1992 151. Ryan A: A dangerous interpretation. Phys Sportsmed 7:43, 1979 152. Laws and regulations pertaining to physical education. Boston, Massachusetts Department of Education; 1978 153. Public Law 94–142; 1977 154. Wichmann S, Martin D: Single-organ patients. Phys Sportsmed 20:176, 1992 155. Tillman W: The patient's right to participate in life. J Am Soc Ocularists 20:29, 1989 156. Woods TA: Ophthalmic lenses for athletes and sportsmen. Optom Clin 3:33, 1993 157. Vinger P: A practical guide for sports eye protection. Phys Sportsmed 28:49, 2000 158. Marmor MF: Double fault! Ocular hazards of a tennis sunglass. Arch Ophthalmol 119:1064, 2001 159. Young RW: Solar radiation and age-related macular degeneration. Surv Ophthalmol 32:252, 1988 160. West SK, Rosenthal FS, Bressler NM, et al: Exposure to sunlight and other risk factors for age-related macular
degeneration. Arch Ophthalmol 107:875, 1989 161. Bressler NM, Bressler SB, West SK, et al: The grading and prevalence of macular degeneration in Chesapeake Bay watermen. Arch Ophthalmol 107:847, 1989 162. Cruickshanks KJ, Klein R, Klein BE, et al. Sunlight and the 5-year incidence of early age-related maculopathy: the
beaver dam eye study. Arch Ophthalmol 119:246, 2001 163. West SK, Duncan DD, Munoz B, et al: Sunlight exposure and risk of lens opacities in a population-based
study: the Salisbury Eye Evaluation project. JAMA 280:714, 1998 164. Taylor HR, West SK, Rosenthal FS, et al: Effect of ultraviolet radiation on cataract formation. N Engl J Med 319:1429, 1988 165. Delcourt C, Carriere I, Ponton-Sanchez A, et al: Light exposure and the risk of cortical, nuclear, and posterior subcapsular
cataracts: the Pathologies Oculaires Liees a l'Age (POLA) study. Arch Ophthalmol 118:385, 2000 166. Bochow TW, West SK, Azar A, et al: Ultraviolet light exposure and risk of posterior subcapsular cataracts. Arch Ophthalmol 107:369, 1989 167. Sliney DH: Epidemiological studies of sunlight and cataract: the critical factor or
ultraviolet exposure geometry. Ophthalmic Epidemiol 1:107, 1994 168. Taylor HR: The biological effects of UV-B on the eye. Photochem Photobiol 50:489, 1989 169. Threlfall TJ, English DR: Sun exposure and pterygium of the eye: a dose-response curve. Am J Ophthalmol 128:280, 1999 170. Taylor HR, West SK, Rosenthal FS, et al: Corneal changes associated with chronic UV irradiation. Arch Ophthalmol 107:1481, 1989 171. Tucker MA, Shields JA, Hartge P, et al: Sunlight exposure as risk factor for intraocular malignant melanoma. N Engl J Med 313:789, 1985 172. Seddon JM, Gragoudas ES, Glynn RJ, et al: Host factors, UV radiation, and risk of uveal melanoma. A case-control
study. Arch Ophthalmol 108:1274, 1990 173. Davis J: Sun and active patients. Phys Sportsmed 28:79, 2000 174. Gilchrest BA, Eller MS, Geller AC, et al: The pathogenesis of melanoma induced by ultraviolet radiation. N Engl J Med 340:1341, 1999 175. Sadun AC, Sadun AA, Sadun LA: Solar retinopathy. A biophysical analysis. Arch Ophthalmol 102:1510, 1984 176. Gladstone GJ, Tasman W: Solar retinitis after minimal exposure. Arch Ophthalmol 96:1368, 1978 177. Sliney DH: Intense light, ultraviolet radiation, and sunglasses. Dispensing Optician May:7, 1985 178. Sliney DH: Eye protective techniques for bright light. Ophthalmology 90:937, 1983 179. Goldstone R: Beware of mirrored sunglasses. Phys Sportsmed 13:16, 1985 180. Mainster MA: The spectra, classification, and rationale of ultraviolet-protective
intraocular lenses. Am J Ophthalmol 102:727, 1986 181. Rosenthal FS, Phoon C, Bakalian AE, et al: The ocular dose of ultraviolet radiation to outdoor workers. Invest Ophthalmol Vis Sci 29:649, 1988 182. Rosenthal FS, Bakalian AE, Lou CQ, et al: The effect of sunglasses on ocular exposure to ultraviolet radiation. Am J Public Health 78:72, 1988 183. Magnante DB, Miller D: Ultraviolet absorption of commonly used clip-on sunglasses. Ann Ophthalmol 17:614, 1985 184. Werner JS: Children's sunglasses: caveat emptor. Optom Vis Sci 68:318, 1991 185. Borgwardt B, Fishman GA, Vander-Meulen D: Spectral transmission characteristics of tinted lenses. Arch Ophthalmol 99:293, 1981 186. Ross D: Ophthalmic lenses: accurately characterizing transmittance of photochromic
and other common lens materials. Appl Optics 30:3673, 1991 187. Weis DR: Contact lenses for athletes. Int Ophthalmol Clin 21:139, 1981 188. Kluka DA, Love PA: The effects of daily-wear contact lenses on contrast sensitivity
in selected professional and collegiate female tennis players. J Am Optom Assoc 64:182, 1993 189. Walker J: SoftPerm for athletes. Spectrum March:55, 1990 190. Spinell MR: Contact lenses for athletes. Optom Clin 3:57, 1993 191. Katz H, Malin A: A new lens for sports proves an excellent troubleshooter. Spectrum March:27, 1990 192. Lichtman W: A new contact lens for athletes. Spectrum August:53, 1991 193. Zuccaro V: Ice hockey and low-water contact lenses. Sports Vision 8:19, 1992 194. Clarke C: Contact lenses at high altitude: experience on Everest south-west
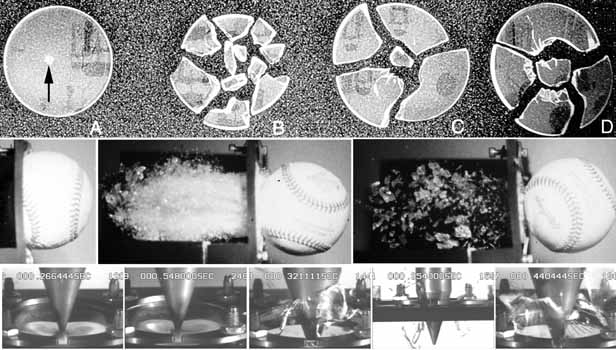
face 1975. Br J Ophthalmol 60:479, 1976 195. Pizzo CJ, Smith WE: Use of contact lenses on mountaineering expeditions. JAMA 252:2701, 1984 196. Butler FK, Jr: . The eye at altitude. Int Ophthalmol Clin 39:59, 1999 197. Bratton SL, Dowd MD, Brogan TV, et al: Serious and fatal air gun injuries: more than meets the eye. Pediatrics 100:609, 1997 198. Endo S, Ishida N, Yamaguchi T: The BB gun is equivalent to the airsoft gun in the Japanese literature. Arch Ophthalmol 118:732, 2000 199. Marshall DH, Brownstein S, Addison DJ, et al: ir guns: the main cause of enucleation secondary to trauma in children
and young adults in the greater Ottawa area in 1974–93. Can J Ophthalmol 30:187, 1995 200. LaRoche GR: Air gun injuries to the eye in children: Canadian ophthalmologists have
to stop the onslaught. Can J Ophthalmol 30:177, 1995 201. USEIR. Selected data. 1988–2001 202. Bond SJ, Schnier GC, Miller FB: Air-powered guns: too much firepower to be a toy. J Trauma 41:674, 1996 203. Enger C, Schein OD, Tielsch JM: Risk factors for ocular injuries caused by air guns. Arch Ophthalmol 114:469, 1996 204. Schein OD, Enger C, Tielsch JM: The context and consequences of ocular injuries from air guns. Am J Ophthalmol 117:501, 1994 205. Naude GP, Bongard FS: From deadly weapon to toy and back again: the danger of air rifles. J Trauma 41:1039, 1996 206. Harris W, Luterman A, Curreri PW: BB and pellet guns—toys or deadly weapons? J Trauma 23:566, 1983 207. Fackler ML: Velocity and air gun injuries. Ann Emerg Med 27:269, 1996 208. Joseph DP, Meredith TA: A new BB forceps. Arch Ophthalmol 118:1574, 2000 209. Brown GC, Tasman WS, Benson WE: BB-gun injuries to the eye. Ophthalmic Surg 16:505, 1985 210. Shanon A, Feldman W: Serious childhood injuries caused by air guns. CMAJ 144:723, 1992 211. Mieler W, Suson J, Williams D: Retained intraocular BB and shotgun foreign bodies. Paper presented at: Scientific Poster 249, 1992; Dallas, TX 212. Kreshon MJ: Eye injuries due to BB guns. Am J Ophthalmol 58:858, 1964 213. Bowen D, Magauran D: Ocular injuries caused by airgun pellets: an analysis of 105 cases. BMJ 1:333, 1973 214. Currie D: Eye injuries from Christmas toys. Sightsaving Rev 26:2, 1956 215. Klopfer J, Tielsch JM, Vitale S, et al: Ocular trauma in the United States. Eye injuries resulting in hospitalization, 1984 through 1987. Arch Ophthalmol 110:838, 1992 216. Martin DF, Meredith TA, Topping TM, et al: Perforating (through-and-through) injuries of the
globe. Surgical results with vitrectomy. Arch Ophthalmol 109:951, 1991 217. LaRoche GR, McIntyre L, Schertzer RM: Epidemiology of severe eye injuries in childhood. Ophthalmology 95:1603, 1988 218. Christoffel KK, Tanz R, Sagerman S, et al: Childhood injuries caused by nonpowder firearms. Am J Dis Child 138:557, 1984 219. Blocker S, Coln D, Chang JH: Serious air rifle injuries in children. Pediatrics 69:751, 1982 220. Shuttleworth GN, Galloway PH: Ocular air-gun injury: 19 cases. J R Soc Med 94:396, 2001 221. Sternberg P Jr.: , de Juan E Jr.: , Green WR, et al: Ocular BB injuries. Ophthalmology 91:1269, 1984 222. Portis JM, Vassallo SA, Albert DM: Ocular sports injuries: a review of cases on file in the Massachusetts
eye and ear infirmary pathology laboratory. Int Ophthalmol Clin 21:1, 1981 223. Pacio CI, Murphy MA: BB embolus causing monocular blindness in a 9-year-old boy. Am J Ophthalmol 134:776, 2002 224. Damore DT, Ramundo ML, Hanna JP, et al: Parental attitudes toward BB and pellet guns. Clin Pediatr 39:281, 2000 225. National Rifle Association: Firearm safety training programs. Washington, D.C.: National Rifle Association Education and Training Division; 2002. 226. American Academy of Ophthalmology: Public Health Note: BB and pellet guns
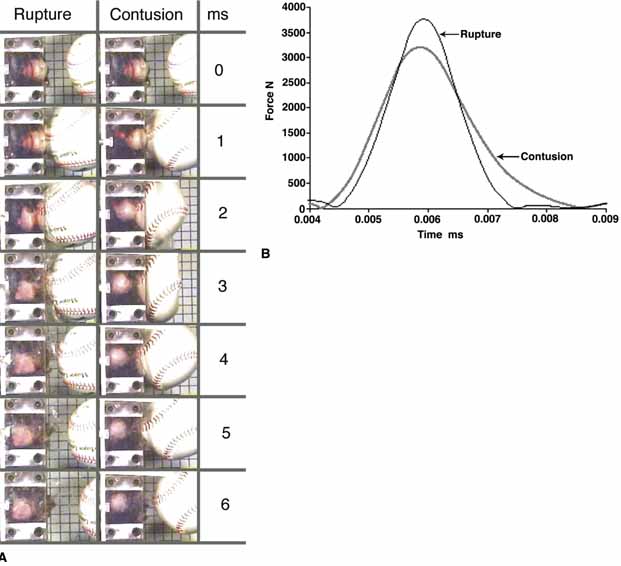
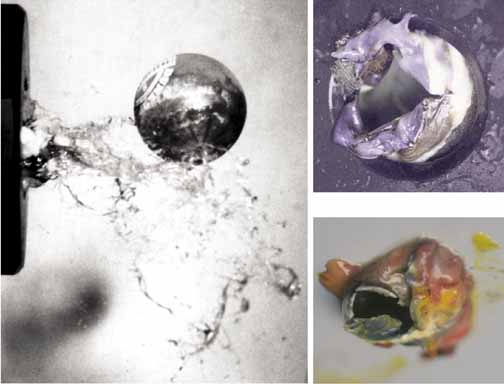
are a major cause of devastating ocular injuries in children. San Francisco: American Academy of Ophthlmology, 1992. 227. Newman TL, Russo PA: Ocular sequelae of BB injuries to the eye and surrounding adnexa. J Am Optom Assoc 69:583, 1998 228. Pulido JS, Gupta S, Folk JC, et al: Perforating BB gun injuries of the globe. Ophthalmic Surg Lasers 28:625, 1997 229. Dinkel TA, Ward TP, Frey DM, et al: Dissection along the optic nerve axis by a BB. Arch Ophthalmol 115:673, 1997 230. Tanz RR, Christoffel KK: Ocular BB injuries. Ophthalmology 92:984, 1985 231. Rudd JC, Jaeger EA, Freitag SK, et al: Traumatically ruptured globes in children. J Pediatr Ophthalmol Strabismus 31:307, 1994 232. The Education and Training Division, National Rifle Association of America: The
Effective Shooting Coach. Washington, D.C.: 1987. 233. Sheets W, Vinger P: Ocular injuries from air guns. Int Ophthalmol Clin 28:225, 1988 234. Ceylan H, McGowan A, Stringer MD: Air weapon injuries: a serious and persistent problem. Arch Dis Child 86:234, 2002 235. Jones LF, III , Classe JG, Hester M, et al: Association between eye dominance and training for rifle marksmanship: a
pilot study. J Am Optom Assoc 67:73, 1996 236. Landers D: Moving competitive shooting into the scientist's lab. American Rifleman April:36, 1980 237. Daniels F: Do the eyes have it? American Rifleman. March:38, 1981 238. Gregg JR: How to prescribe for hunters and marksmen. J Am Optom Assoc 51:675, 1980 239. Breedlove HW: Prescribing for marksmen and hunters. Optom Clin 3:77, 1993 240. Pomeranz R: Shooting glasses: what color's best? American Rifleman July:28, 1991 241. Dannenberg AL, Parver LM, Fowler CJ: Penetrating eye injuries related to assault. The National Eye Trauma System
Registry. Arch Ophthalmol 110:849, 1992 242. Kellermann AL, Rivara FP, Lee RK, et al: Injuries due to firearms in three cities. N Engl J Med 335:1438, 1996 243. Blendon RJ, Young JT, Hemenway D: The American public and the gun control debate. JAMA 275:1719, 1996 244. Hemenway D, Solnick SJ, Azrael DR: Firearm training and storage. JAMA 273:46, 1995 245. From the Centers for Disease Control and Prevention: Hunting-associated
injuries and wearing “hunter” orange clothing—New
York, 1989–1995. JAMA 276:1462, 1996 246. Hunting-associated injuries and wearing “hunter” orange
clothing—New York, 1989–1995. MMWR Morb Mortal Wkly Rep 45:884, 1996 247. Alfaro DV, Tran VT, Runyan T, et al: Vitrectomy for perforating eye injuries from shotgun pellets. Am J Ophthalmol 114:81, 1992 248. Ford JG, Barr CC: Penetrating pellet fragmentation. A complication of ocular shotgun injury. Arch Ophthalmol 108:48, 1990 249. Danesh-Meyer HV, Savino PJ, Bilyk JR, et al: Gaze-evoked amaurosis produced by intraorbital buckshot pellet. Ophthalmology 108:201, 2001 250. Agbeja AM, Osuntokun O: Ocular gun-shot injuries in Ibadan. Afr J Med Med Sci 20:35, 1991 251. McIntyre MW: Bilateral gunshot perforations with retention of useful vision: a case
report. Eye Ear Nose Throat Mon 48:567, 1969 252. Dreizen NG, Stulting RD: Ocular gunpowder injuries. Am J Ophthalmol 100:852, 1985 253. Runyan TE, Ewald RA: Blank cartridge injury of the cornea. Arch Ophthalmol 84:690, 1970 254. Simmons ST, Krohel GB, Hay, PB: Prevention of ocular gunshot injuries using polycarbonate lenses. Ophthalmology 91:977, 1984 255. Varr WF, III , Cook RA: Shotgun eye injuries. Ocular risk and eye protection efficacy. Ophthalmology 99:867, 1992 256. Department of Defense: Department of Defense Test Method sSandard: V50 Basllistic test for armor. MIL-STD–662E. Washington, D.C.: Department of Defense, 1997 257. Krishnamachary M, Rathi V, Gupta S: Management of traumatic cataract in children. J Cataract Refract Surg 23(Suppl 1):681, 1997 258. Dasgupta S, Mukherjee R, Ladi DS, et al: Pediatric ocular trauma—a clinical presentation. J Postgrad Med 36:20, 1990 259. Takvam JA, Midelfart A: Survey of eye injuries in Norwegian children. Acta Ophthalmol (Copenh) 71:500, 1993 260. Mono J, Hollenberg RD, Harvey JT: Occult transorbital intracranial penetrating injuries. Ann Emerg Med 15:589, 1986 261. Paucic-Kirincic E, Prpic I, Gazdik M, et al: Transorbital penetrating brain injury caused by a toy arrow: a case report. Pediatr Rehabil 1:191, 1997 262. Hornblass A: Ocular war injuries in South Vietnam. Surg Forum 24:500, 1973 263. Hornblass A: Eye injuries in the military. Int Ophthalmol Clin 21:121, 1981 264. Belkin M: Ocular injuries in the Yom Kippur war. J Ocuk Ther Surg Jan-Feb:40, 1983 265. Mader TH, Aragones JV, Chandler AC, et al: Ocular and ocular adnexal injuries treated by United States military ophthalmologists
during Operations Desert Shield and Desert Storm. Ophthalmology 100:1462, 1993 266. Heier JS, Enzenauer RW, Wintermeyer SF, et al: Ocular injuries and diseases at a combat support hospital in support of
Operations Desert Shield and Desert Storm. Arch Ophthalmol 111:795, 1993 267. Belkin M, Treister G, Dotan S: Eye injuries and ocular protection in the Lebanon War, 1982. Isr J Med Sci 20:333, 1984 268. US Department of Defens: National mortality profile of active duty personnel
in the U.S. armed forces: 1980–1993. Cincinnati, OH: National Institute for Occupational Safety and Health, 1996. 269. Andreotti G, Lange JL, Brundage JF: The nature, incidence, and impact of eye injuries among US military personnel: implications
for prevention. Arch Ophthalmol 119:1693, 2001 270. Tengroth BM: Laser weapons designed to produce blindness. Am J Ophthalmol 116:370, 1993 271. Thomas SR: Aircrew laser eye protection: visual consequences and mission performance. Aviat Space Environ Med 65(5 Suppl):A108, 1994 272. Gillow JT: Another weapon too far: the anti-personnel laser. J R Soc Med 88:347P, 1995 273. Tengroth B: [Ban the laser weapons! Invisible rays may cause permanent blindness
in thousands of war victims]. Lakartidningen 92:837, 1995 274. Wong TY, Seet MB, Ang CL: Eye injuries in twentieth century warfare: a historical perspective. Surv Ophthalmol 41:433, 1997 275. Cotter F, La Piana FG: Eye casualty reduction by eye armor. Mil Med 156:126, 1991 276. LaPiana FG: The development of eye armor for the American infantryman. Washington, D.C.: Department of the Army, Walter Reed Army Medical Center, 1989 277. Blakeslee S: Eye armor, blindness prevention in the military. Sightsaving 55:4, 1986 278. Ward DL, Gorie C: Occupational eye injuries in soldiers. J Occup Med 33:646, 1991 279. Lipscomb HJ: Effectiveness of interventions to prevent work-related eye injuries. Am J Prev Med 18(4 Suppl):27, 2000 280. Blais B: Basic Principles of industrial ophthalmology. Ophthalmol Clin North Am 13:309, 2000 281. Carter GC: ASTM helps modern fencing stay modern: protect those heads. ASTM Stand News October:56, 1985 282. Sotiropoulos SV, Jackson MA, Tremblay GF, et al: Childhood lawn dart injuries. Summary of 75 patients and patient report. Am J Dis Child 144:980, 1990 283. Cole MD, Smerdon D: Perforating eye injuries caused by darts. Br J Ophthalmol 72:511, 1988 284. Patel BC, Morgan LH: Serious eye injuries caused by darts. Arch Emerg Med 8:289, 1991 285. Thill-Schwaninger M, Marquardt R: [Perforating eye injuries caused by darts]. Klin Monatsbl Augenheilkd 192:699, 1988 286. Bastrikov NI: [Tactics for extricating a fishing hook from the eye and its adnexa]. Vestn Oftalmol 102:67, 1986 287. Krott R, Bartz-Schmidt KU, Heimann K: Laceration of the eye with a fishing hook. Br J Ophthalmol 83:1194, 1999 288. Petrovic Z, Krstic L: [Surgery of an eye injury caused by a fishing hook]. Vojnosanit Pregl 38:267, 1981 289. Bialasiewicz AA, Fuisting B, Schwartz R, et al: [Severe ocular injuries caused by fishing equipment]. Klin Monatsbl Augenheilkd 214:27, 1999 290. Coden DJ: Ruptured globe caused by a fishing sinker. Arch Ophthalmol 120:407, 2002 291. Erisen L, Basut O, Coskun H, et al: An unusual penetrating facial injury due to a fishing-line sinker. J Oral Maxillofac Surg 59:945, 2001 292. Katsumata S, Takahashi J, Tamai M: Chorioretinitis sclopetaria caused by fishing line sinker. Jpn J Ophthalmol 28:69, 1984 293. Malhotra R, Tappin M, Olver JM: Angler's fishing line sinker causing rupture of globe and medial wall
fracture. Eye 13(Pt 2):260, 1999 294. Zeligowski AA, Ilsar M, Berger S, et al: Eye injuries induced by a barbed three-pronged fishing spear. Arch Ophthalmol 104:639, 1986 295. Hefer T, Joachims HZ, Loberman Z, et al: [Facial injury by fishing harpoons]. Harefuah 127:295, 1994 296. Raynor LA: Eye protection for anglers. N Engl J Med 307:954, 1982 297. Endo S, Ishida N, Yamaguchi T: Tear in the trabecular meshwork caused by an airsoft gun. Am J Ophthalmol 131:656, 2001 298. Fleischhauer JC, Goldblum D, Frueh BE, et al: Ocular injuries caused by airsoft guns. Arch Ophthalmol 117:1437, 1999 299. American National Standards Institute: American National Standard Practice
for Occupational and Educational Personal Eye and Face Protective
Devices. ANSI Z87.1–89 R1998. New York: American National Standards Institute, Inc., 1998 300. Vinger PF, Jeffers JB, McGuire RC, et al: Paintball eye injuries: the changing of an industry. Int J Sports Vis 7:30, 2001 301. Vinger P, Sparks J, Mussack K, et al: A program to prevent eye injuries in paintball. Sports Vis 3:33, 1997 302. Kitchens JW, Danis RP: Increasing paintball related eye trauma reported to a state eye injury
registry. Inj Prev 5:301, 1999 303. Easterbrook M, Pashby TJ: Ocular injuries and war games. Int Ophthalmol Clin 28:222, 1988 304. Morgan B: Director, Product Development, Titleist. Fairhaven. MA: Personal Communication, 1993. 305. Mulvihill A, O'Sullivan J, Logan P: Penetrating eye injury caused by a golf tee. Br J Ophthalmol 81:91, 1997 306. Millar GT: Golfing eye injuries. Am J Ophthalmol 64:741, 1967 307. Mieler WF, Nanda SK, Wolf MD, et al: Golf-related ocular injuries. Arch Ophthalmol 113:1410, 1995 308. Brennan PO: Golf related head injuries in children. BMJ 303:54, 1991 309. Galler E, Umlas J, Vinger P, et al: Ocular integrity after quantitated trauma following photorefractive keratectomy
and automated lamellar keratectomy, 1995; Arvo Ft. Laurderdale, FL. 310. Umlas J, Galler E, Vinger P, et al: Ocular integrity after quantitated trauma in radial keratotomy eyes., 1995; Arvo Ft. Laurderdale, FL. 311. Slusher MM, Jaegers KR, Annesley WH Jr. : Liquid-center golf balls and ocular injury. Am J Ophthalmol 64:736, 1967 312. Kunkel RE: Exploding golf balls. Rocky Mt Med J 64:82, 1967 313. Nelson C: Eye injury from exploding golf balls. Br J Ophthalmol 54:670, 1970 314. Farley KG: Ocular trauma resulting from the explosive rupture of a liquid center golf
ball. J Am Optom Assoc 56:310, 1985 315. O'Grady R, Shoch D: Golf-ball granuloma of the eyelids and conjunctiva. Am J Ophthalmol 76:148, 1973 316. Penner R: The liquid center golf ball: a potential ocular hazard. Arch Ophthalmol 75:68, 1966 317. Lucas DR, Dunham AC, Lee WR, et al: Ocular injuries from liquid golf ball cores. Br J Ophthalmol 60:740, 1967 318. Ishii Y, Inoue S, Kikuchi I, et al: Barium granuloma. YJ Dermatol 9:153, 1982 319. Johnson FB, Zimmerman LE: Barium sulfate and zinc sulfide deposits resulting from golf-ball
injury to the conjunctiva and eyelid. Am J Clin Pathol 44:533, 1965 320. Burnstine MA, Elner VM: Golf-related ocular injuries. Am J Ophthalmol 121:437, 1996 321. Pashby T: Eye injuries in Canadian sports and recreation, 1972–2002. Can J Ophthalmol 37:253, 2002 322. Jones NP: Eye injuries in sport: an increasing problem. Br J Sports Med 21:168, 1987 323. Baller R: Racquet Sports Injuries. Bloomington, IL: University of Illinois, 1979 324. Barrell GV, Cooper PJ, Elkington AR, et al: Squash ball to eye ball: the likelihood of squash players incurring an
eye injury. Br Med J (Clin Res Ed) 283:893, 1981 325. Easterbrook M: Eye injuries in racket sports. Int Ophthalmol Clin 21:87, 1981 326. Easterbrook M: Ocular injuries in racquet sports. Int Ophthalmol Clin 28:232, 1988 327. Doxanas MT, Soderstrom C: Racquetball as an ocular hazard. Arch Ophthalmol 98:1965, 1980 328. Vinger PF, Tolpin DW: Racket sports. An ocular hazard. JAMA 239:2575, 1978 329. Kaplan P: The sight you save. Family Health April:34, 1979 330. Feigelman MJ, Sugar J, Jednock N, et al: Assessment of ocular protection for racquetball. JAMA 250:3305, 1983 331. Bishop P, Kozey J, Caldwell G: Performance of eye protectors for squash and racquetball. Phys Sportsmed 10:63, 1982 332. Morehouse C: Preliminary Evaluation of Eye Protective Devices for Racquet Sports. University Park, PA: Sports Research Institute, Pennsylvania State University, 1983 333. ASTM. Standard Specification for Eye Protectors for Selected Sports. ASTM F803. West Conshohocken, PA: American Society for Testing and Materials, 2001 334. Easterbrook M: Eye injuries in squash and racquetball players: an update. Phys Sportsmed 10:47, 1982 335. Cooper A: Your eyeguards may not protect you. Handball 39:7, 1989 336. Turriff T: Handball association scores points for eye safety. National Society to
Prevent Blindness, Update. 36:1, 1986 337. Ingram DV, Lewkonia I: Ocular hazards of playing squash rackets. Br J Ophthalmol 57:434, 1973 338. North IM: Ocular hazards of squash. Med J Aust. 1:165, 1973 339. Jean D, Detry-Morel M: Stellar corneal rupture and secondary glaucoma after squash trauma in a
keratotomized eye. Bull Soc Belge Ophtalmol 245:109, 1992 340. Sabiston D: Squash and eye injuries. N Z J Sports Med 4:3, 1976 341. Knorr HL, Jonas JB: Retinal detachments by squash ball accidents. Am J Ophthalmol 122:260, 1996 342. Clemett RS, Fairhurst SM: Head injuries from squash: a prospective study. N Z Med J 92:1, 1980 343. Reif A, Vinger P, Easterbrook M: New developments in protection against eye injuries. Squash News 4:10, 1981 344. Genovese MT, Lenzo NP, Lim RK, et al: Eye injuries among pennant squash players and their attitudes towards protective
eyewear. Med J Aust 153:655, 1990 345. Finch C, Vear P: What do adult squash players think about protective eyewear? Br J Sports Med 32:155, 1998 346. Pipes T: The racquetball pro: a physiologic profile. Phys Sportsmed 7:91, 1979 347. Rose C, Morse J: Racquetball injuries. Phys Sportsmed 1979;7:73–78. 348. Soderstrom C, Doxanas MT: Racquetball: a game with preventable injuries. Am J Sports Med 10:180, 1982 349. Chandran S: Hyphaema and badminton eye injuries. Med J Malaya 26:207, 1972 350. Labelle P, Mercier M, Podtetenev M, et al: Eye injuries in sports: results of a five year study. Phys Sportsmed 16:126, 1988 351. Kelly SP: Serious eye injury in badminton players. Br J Ophthalmol 71:746, 1987 352. Chandran S: Ocular hazards of playing badminton. Br J Ophthalmol 58:757, 1974 353. Ryan A: Eye protection for athletes: a round table discussion. Phys Sportsmed 6:44, 1978 354. Easterbrook M: Prevention of eye injuries in badminton. In Hermans G, ed. Sports Medicine and Health. New York: Elsevier Science Publishers, 1990:1107–1110 355. McWhae J, LaRoche GR: Badminton-related eye injuries. Can J Ophthalmol 25:170, 1990 356. Hensley LD, Paup DC: A survey of badminton injuries. Br J Sports Med 13:156, 1979 357. Holter NJ: Tennis balls and eye injuries. JAMA 237:1312, 1977 358. Vinger PF, Parver L, Alfaro DV, III , et al: Shatter resistance of spectacle lenses. JAMA 277:142, 1997 359. Vinger PF: The incidence of eye injuries in sports. Int Ophthalmol Clin 21:21, 1981 360. Seelenfreund MH: Tennis players and eye injuries. JAMA 236:2287, 1976 361. Duke M: Tennis players and eye injuries. JAMA 236:2287, 1976 362. Seelenfreund M: Reply to letter from Duke, M. JAMA 236:2287, 1976 363. Koch P: Delighted with results of his RK, surgeon schooled in pain, glare. Ocular Surg News 10:4, 1992 364. Koch P: Presentation. Paper presented at: New England Ophthalmological Society. Boston, MA: 1992 365. Moore M: Fighting NHL brawling with suspensions. Phys Sportsmed 8:19, 1980 366. Reeves J, Mendryk S: Greater Edmonton metropolitan area hockey injury study: Department of Physical
Education, University of Alberta, Alberta Safety Council; 1969–70 367. Hornof Z, Napravnik C: Analysis of various accident rate factors in ice hockey. Med Sci Sports 5:283, 1973 368. Accidents associated with hockey equipment. Washington, D.C.: US Consumer Product Safety Commission, Bureau of Epidemiology, 1973. 369. Muller P, Biener K: [Sport accidents in ice hockey]. Munch Med Wochenschr 115:564, 1973 370. Biener K, Muller P: [Ice-hockey accidents]. Cah Med 14:959, 1973 371. Park R, Castaldi CR: Injuries in junior ice hockey. Phys Sportsmed 8:81, 1980 372. Sim FH, Simonet WT, Melton LJ, III , et al: Ice hockey injuries. Am J Sports Med 15:30, 1987 373. Rontal E, Rontal M, Wilson K, et al: Facial injuries in hockey players. Laryngoscope 87:884, 1977 374. Wilson K, Cram B, Rontal E, et al: Facial injuries in hockey players. Minn Med 6013, 1977 375. Hastings D, Cameron J, Parker S, et al: A study of hockey injuries in Ontario. Ont Med Rev November:686–692, 1974 376. Pashby TJ, Pashby RC, Chisholm LD, et al: Eye injuries in Canadian hockey. Can Med Assoc J 113:663, 1975 377. Castaldi CR: Connecticut's new mandatory face guard rule. U.S. Hockey/Arena Biz. 4:5, 1976 378. Horns RC: Blinding hockey injuries. Minn Med 59:255, 1976 379. Vinger PF: Ocular injuries in hockey. Arch Ophthalmol 94:74, 1976 380. Vinger P: Hockey facial injuries. Massachusetts Secondary School Principals' Association Bugle. June 7, 1975 381. Antaki S, Labelle P, Dumas J: Retinal detachment following hockey injury. Can Med Assoc J 117:245, 1977 382. Feriencik K: Trends in ice hockey injuries: 1965 to 1977. Phys Sportsmed 7:81, 1979 383. Dyment P: Violence in youth hockey. Phys Sportsmed 17:55, 1989 384. Hayes D: Hockey injuries: how, why, where, and when? Phys Sportsmed 3:61, 1975 385. Vinger P: 1976 report on facial injuries in hockey. Boston: Massachusetts Secondary Schools Principals Association, 1976 386. Pashby TJ: Eye injuries in Canadian hockey. Phase II. Can Med Assoc J 117:671, 1977 387. Capillo J: Hockey masks go on, face injuries go down. Phys Sportsmed 5:77, 1977 388. Downs J: Incidence of facial trauma in intercollegiate and junior hockey. Phys Sportsmed 7:88, 1979 389. Pashby T: Eye injuries in Canadian amateur hockey. Can J Ophthalmol 20:2, 1985 390. Pashby TJ: Eye injuries in Canadian hockey. Phase III: Older players now most at risk. Can Med Assoc J 121:64, 1979 391. Lorentzon R, Wedren H, Pietila T, et al: Injuries in international ice hockey. A prospective, comparative study
of injury incidence and injury types in international and Swedish elite
ice hockey. Am J Sports Med 16:389, 1988 392. Lorentzon R, Wedren H, Pietila T: Incidence, nature, and causes of ice hockey injuries. A three-year prospective study of a Swedish elite ice hockey team. Am J Sports Med 16:392, 1988 393. Castaldi CR: 1976–1977 New England A.H.A. experiences with facial protective equipment: report
of the chairman. Farmington: Safety and Protective Equipment Committee of the Connecticut Hockey Conference (AHAUS); March 15, 1977 394. Sim FH, Simonet WT: Ice hockey injuries. Phys Sportsmed 16:92, 1988 395. Pashby T: Eye injuries in Canadian amateur hockey still a concern. Can J Ophthalmol. 22:293, 1987 396. Castaldi CR: Sports-related oral and facial injuries in the young athlete: a
new challenge for the pediatric dentist. Pediatr Dent 8:311, 1986 397. Castaldi CR: Prevention of craniofacial injuries in ice hockey. Dent Clin North Am 35:647, 1991 398. Sane J, Ylipaavalniemi P, Leppanen H: Maxillofacial and dental ice hockey injuries. Med Sci Sports Exerc 20:202, 1988 399. Lahti H, Sane J, Ylipaavalniemi P: Dental injuries in ice hockey games and training. Med. Sci. Sports Exerc 34:400, 2001 400. Smith T, Bishop P: Impact of full face and visor type hockey face guards. In Castaldi C, Hoerner E, eds. Safety in Ice Hockey. Vol STP 1050. Philadelphia: ASTM, 1989:235–239 401. Sze Y, Thomson J, Norman R, et al: Procedures for the evaluation of hockey goaltender's face masks. In Bleustein J, ed. Mechanics and Sports. New York: American Society of Mechanical Engineers, 1973:175–181 402. Rovere G, Gristina A, Nicastro J: Medical problems of a professional hockey team: a three season experience. Phys Sportsmed 6:59, 1978 403. Hache A: The Physics of Hockey. Baltimore: The Johns Hopkins University Press, 2002 404. Norman R, Thomsoon J, Sze Y, et al: Relative impact attenuating properties of face masks of ice hockey goaltenders. In Nelson R, Morehouse C, eds. Biomechanics IV. Baltimore: University Park Press, 1974 405. Galbraith RF: Safety in hockey: cage versus molded masks for goalies, protective helmets
for referees. Minn Med 64:671, 1981 406. Regnier G, Sicard C, Goulet C: Economic impact of a regulation imposing full face protectors on adult
recreational hockey players. Int J Consumer Safety 2:191, 1995 407. Tolpin H, Bentkover J: The economic costs of sports injuries. In Vinger P, Hoerner E, eds. Sports Injuries: The Unthwarted Epidemic. Littleton, MA: PSG Publishing Co., Inc., 1981:45–55. 408. Dryden DM, Francescutti LH, Rowe BH, et al: Epidemiology of women's recreational ice hockey injuries. Med Sci Sports Exerc 32:1378, 2000 409. Marton K, Wilson D, McKeag D: Ocular trauma in college varsity sports. Med Sci Sports Exerc 19(April suppl):S53, 1987 410. LaPrade RF, Broxterman R: The single strap helmet fixation system in intercollegiate ice hockey: a
source of variable face protection. In Ashare A, ed. Safety in Ice Hockey: Third Volume. West Conshohocken, PA: ASTM STP 1341; 2000:124–129 411. Vinger P: Eye and faced protection for United States hockey players: a chronology. In Vinger P, ed. International Ophthalmology Clinics: Ocular Sports Injuries. Vol. 21. Boston: Little, Brown and Company, 1981:83–86 412. Hayes D: Reducing risks in hockey: analysis of equipment and injuries. Phys Sportsmed 6:67, 1978 413. Tator CH, Carson JD, Edmonds VE: Spinal injuries in ice hockey. Clin Sports Med 17:183, 1998 414. Tator CH: Neck injuries in ice hockey: a recent, unsolved problem with many contributing
factors. Clin Sports Med 6:101, 1987 415. Tator CH, Carson JD, Cushman R: Hockey injuries of the spine in Canada, 1966–1996. CMAJ 162:787, 2000 416. Tator CH, Carson JD, Edmonds VE: New spinal injuries in hockey. Clin J Sport Med 7:17, 1997 417. Tator CH, Edmonds VE: National survey of spinal injuries in hockey players. Can Med Assoc J 130:875, 1984 418. Tator CH, Edmonds VE, Lapczak L, et al: Spinal injuries in ice hockey players, 1966–1987. Can J Surg 34:63, 1991 419. Tator CH, Ekong CE, Rowed DW, et al: Spinal injuries due to hockey. Can J Neurol Sci 11:34, 1984 420. Murray TM, Livingston LA: Hockey helmets, face masks, and injurious behavior. Pediatrics 95:419, 1995 421. Stoner L, Keating M: Hockey equipment: safety or an illusion? In Castaldi CR, Bishop P, Hoerner E, eds. Safety in Ice Hockey: Second volume. Vol. STP 1212. Philadelphia: ASTM, 1993:183–191 422. Walsh S: A proposal for the use of the half face, clear plastic visor for National
Collegiate Athletic Association hockey. In Castaldi C, Hoerner E, eds. Safety in ice hockey. Philadelphia: ASTM STP 1050; 1989:55–57 423. Bayan G: Reflections on a hockey helmet. Newsweek page 13, March 12, 1984. 424. Vinger P, Bentkover J, Sullivan R, et al: The hockey face guard: health care costs and ethics. In Castaldi C, Hoerner E, eds. Safety in Ice Hockey. Philadelphia: ASTM STP 1050; 1989:58–62 425. Benson BW, Rose MS, Meeuwisse WH: The impact of face shield use on concussions in ice hockey: a multivariate
analysis. Br J Sports Med 36:27, 2002 426. Smith A, Colbenson C, Kronebusch S: A psychosocial perspective of aggression in ice hockey. In Ashare A, ed. Safety in Ice Hockey: Third volume. Philadelphia: ASTM STP 1341; 2000 427. Gaumond S, Trudel P, Gilbert W: Amateur youth ice hockey coaches' views on rule infractions, aggressive
play, and injuries during games. In Ashare A, ed. Safety in Ice hockey: Third volume. Philadelphia: ASTM STP 1341; 2000 428. Swift E: Blood and ice. Sports Illustrated 69:261–273 1988 429. Myles WM, Dickinson JD, LaRoche GR: Ice hockey and spectators' eye injuries. N Engl J Med 329:364, 1993 430. Cotton T: Eye injuries 1978–1979, 1.5 school years. Concord: Concord/Carlisle
Regional School District, 1979 431. Hyman A. Personal communication, 1984 432. Rose C: Injuries in women's field hockey: a four-year study. Phys Sportsmed 9:97, 1981 433. Anonomous: Big Ten requires mouth guards in field hockey. Phys Sportsmed 10:28, 1982 434. Elliott AJ, Jones D: Major ocular trauma: a disturbing trend in field hockey injuries. Br Med J (Clin Res Ed) 289:21, 1984 435. Hodgson V: Personnel communication, 1984. 436. Kuland D, Schildwachter T, McCue F, et al: Lacrosse injuries. Phys Sportsmed 7:82, 1979 437. Nelson W, DePalma B, Gieck J, et al: Intercollegiate lacrosse injuries. Phys Sportsmed 9:86, 1981 438. LeRoy N: Questionable value: a helmet rule has altered girl's lacrosse in Massachusetts
for the worse. Lacrosse 16:8, 1992 439. Hawthorne P: Don't rush to force helmets on women's lacrosse. Lacrosse Magazine. 17:13, 1993 440. Vinger P: Why women's lacrosse players should wear helmets. Lacrosse Magazine. 17:8, 1993 441. Piltz W: Eye and facial injuries in women's lacrosse: a paper on women's
lacrosse in Australia. Paper presented at: Second International Symposium on Ocular Trauma, Geneva: 1992 442. Lapidus CS, Nelson LB, Jeffers JB, et al: Eye injuries in lacrosse: women need their vision less than men? J Trauma 32:555, 1992 443. Webster DA, Bayliss GV, Spadaro JA: Head and face injuries in scholastic women's lacrosse with and without
eyewear. Med Sci Sports Exerc 31:938, 1999 444. Waicus KM, Smith BW: Eye injuries in women's lacrosse players. Clin J Sport Med 12:24, 2002 445. Piltz W: Report to South Australia Women's Lacrosse Association Board, 1992 446. Massachusetts Interscholastic Athletic Association: Women's Lacrosse
Injury report Data, 1985–1995. Franklin, MA: Massachusetts Interscholastic Athletic Association 447. Hawthorne P: Seeing eye to eye on protection. Women's Lacrosse April/May:1, 1993 448. Livingston LA, Forbes SL: Eye injuries in women's lacrosse: strict rule enforcement and mandatory
eyewear required. J Trauma 40:144, 1996 449. Livingston L, Forbes S: Rules changes, rule enforcement, and ocular injury rates in women's
lacrosse and men's ice hockey. Int J Sports Vis 6:37, 2000 450. Canadian Standards Association: National Standard of Canada (CAN 3-Z262.2-M90) Face Protectors for Ice Hockey and Box
Lacrosse Players. Rexdale, Ontario: Cadanian Standards Association, 1997 451. Harada T, Hirano K, Ishii M, et al: [Evaluation of 164 cases of ocular injuries caused by various sports]. J Fr Ophtalmol 8:455, 1985 452. Napier SM, Baker RS, Sanford DG, et al: Eye injuries in athletics and recreation. Surv Ophthalmol 41:229, 1996 453. Orlando RG, Doty JH: Ocular sports trauma: a private practice study. J Am Optom Assoc 67:77, 1996 454. Caveness LS: Ocular and facial injuries in baseball. Int Ophthalmol Clin 28:238, 1988 455. Forrest LA, Schuller DE, Strauss RH: Management of orbital blow-out fractures. Case reports and discussion. Am J Sports Med 17:217, 1989 456. Rothnaum M, Danis R: Baseball-related eye injuries reported to the Eye Injury Registry. Trauma Times Winter :3, 2001 457. Kyle S: Youth baseball protective equipment project final report. Washington, D.C.: U.S. Consumer Product Safety Commission. May 1996 458. Yen KL, Metzl JD: Sports-specific concerns in the young athlete: baseball. Pediatr Emerg Care 16:215, 2000 459. Schuster M: Baseball-related injuries among children. Boston: Statewide Comprehensive Injury Prevention Program, Bureau of Parent, Child and Adolescent Health, Massachusetts Department of Public Health, 1991 460. Hale C: Statistical report on injuries in Little League baseball. Paper presented
at: American Academy of Orthopedic Surgeons; January 16, 1967 461. Zagelbaum BM, Hersh PS, Donnenfeld ED, et al: Ocular trauma in major-league baseball players. N Engl J Med 330:1021, 1994 462. Hale C: Protective equipment in baseball. Phys Sportsmed 7:59, 1979 463. American Academy of Pediatrics: Risk of injury from baseball and softball
in children 5 to 14 years of age: Statement: Committee on Sports Medicine
and Fitness, American Academy of Pediatrics. Pediatrics 93:690, 1994 464. Parmet S, Lynm C, Glass RM: JAMA patient page. Baseball safety for children. JAMA 289:652, 2003 465. Adair R: The Physics of Baseball. New York: Harper and Row, 1990 466. Seefeldt V, Brown E, WIlson D, et al: Influence of low-compression versus traditional baseballs on injuries
in youth baseball. East Lansing: Institute for the Study of Youth Sport, Michigan State University; July 20, 1993 467. Crisco J, Hendee S, Greenwald R: The influence of baseball modulus and mass on head and chest impacts: a
theoretical study. Med Sci Sports Exerc 29:26, 1997 468. Heald J, Pass D: Ball standards relevant to risk of head injury. Paper presented at: Head
and Neck Injuries in Sports. Philadelphia, PA: 1994. 469. King A, Hodgson V: Comparison of the effect of RIF and major league impacts on the acceleration
response and skull fracture patterns of cadaver heads. Tullahoma, TN: Report to Worth, Inc., December 23, 1992 470. Heald J: Ball standards relevant to risk of head injury. Paper presented at: Head
and Neck Injuries in Sports. Philadelphia: 1994 471. Danis RP, Hu K, Bell M: Acceptability of baseball face guards and reduction of oculofacial injury
in receptive youth league players. Inj Prev 6:232, 2000 472. Marshall SW, Mueller FO, Kirby DP, et al: Evaluation of safety balls and faceguards for prevention of injuries in
youth baseball. JAMA 289:568, 2003 473. Vinger P: Baseball eye protection: the effect of impact by major league and reduced
injury factor baseball on currently available eye protectors. International
Symposium on Safety in Baseball and Softball. Philadelphia In: Hoerner E, Cosgrove F, eds. ASTM STP 1313: 1997:29–37 474. Glassman R: Tradition bound resistance hinders youth baseball safety. Paper presented
at: International Symposium on Safety in Baseball/Softball. Philadelphia: 1997 475. Janda DH, Wojtys EM, Hankin FM, et al: A three-phase analysis of the prevention of recreational softball
injuries. Am J Sports Med 18:632, 1990 476. Adair R: The physics of baseball; the standardization of balls and bats for recreational
softball. Paper presented at: International Symposium on Safety in Baseball and Softball. Philadelphia: 1997 477. Regan D: Visual judgements and misjudgements in cricket, and the art of flight. Perception 21:91, 1992 478. Forward GR: Indoor cricket injuries. Med J Aust 148:560, 1988 479. Jones NP, Tullo AB: Severe eye injuries in cricket. Br J Sports Med 20:178, 1986 480. Aburn N: Eye injuries in indoor cricket at Wellington Hospital: a survey January 1987 to
June 1989. N Z Med J 103:454, 1990 481. Lim LH, Moore MH, Trott JA, et al: Sports-related facial fractures: a review of 137 patients. Aust N Z J Surg 63:784, 1993 482. Coroneo MT: An eye for cricket. Ocular injuries in indoor cricketers. Med J Aust 142:469, 1985 483. Keeney AH: Prevention of eye injuries. In Freeman H, ed. Ocular Trauma. Boston: Appleton-Century-Crofts, 1979:377–383. 484. Orlando R: Soccer-related eye injuries in children and adolescents. Phys Sportsmed 16:103, 1988 485. Horn EP, McDonald HR, Johnson RN, et al: Soccer ball-related retinal injuries: a report of 13 cases. Retina 20:604, 2000 486. Filipe JA, Barros H, Castro-Correia J: Sports-related ocular injuries. A three-year follow-up
study. Ophthalmology 104:313, 1997 487. Drolsum L: Eye injuries in sports. Scand J Med Sci Sports 9:53, 1999 488. Pikkel J, Gelfand Y, Miller B: [Incidence of sports-related eye injuries]. Harefuah. Oct 129:249, 1995 489. Capao Filipe JA, Fernandes VL, Barros H, et al: Soccer-related ocular injuries. Arch Ophthalmol 121:687, 2003 490. Matser JT, Kessels AG, Jordan BD, et al: Chronic traumatic brain injury in professional soccer players. Neurology 51:791, 1998 491. Kirkendall DT, Jordan SE, Garrett WE: Heading and head injuries in soccer. Sports Med 31:369, 2001 492. Reed WF, Feldman KW, Weiss AH, et al: Does soccer ball heading cause retinal bleeding? Arch Pediatr Adolesc Med 156:337, 2002 493. Verdaguer J: Juvenile retinal detachment. Pan American Association of Ophthalmology
and American Journal of Ophthalmology Lecture. Am J Ophthalmol 93:145, 1982 494. Injuries associated with soccer goalposts—United States, 1979–1993. MMWR Morb Mortal Wkly Rep 43:153, 1994 495. Centers for Disease Control and Prevention. Injuries associated with soccer
goalposts—United States, 1979–1993. JAMA 271:1233, 1994 496. Janda DH, Bir C, Wild B, Olson S, et al: Goal post injuries in soccer. A laboratory and field testing analysis of
a preventive intervention. Am J Sports Med 23:340, 1995 497. Apple D: Basketball injuries:an overview. Phys Sportsmed 16:64, 1988 498. Zagelbaum BM, Starkey C, Hersh PS, et al: The National Basketball Association eye injury study. Arch Ophthalmol 113:749, 1995 499. Foster BS, March GA, Lucarelli MJ, et al: Optic nerve avulsion. Arch Ophthalmol 115:623, 1997 500. Chang M, Eifrig DE: Optic nerve avulsion. Case report. Arch Ophthalmol 105:322, 1987 501. Gradin D: Minor trauma can cause major damage. Ophthalmology Times June 5–11:9, 1995 502. Williams DF, Williams GA, Abrams GW, et al: Evulsion of the retina associated with optic nerve evulsion. Am J Ophthalmol 104:5, 1987 503. Panda A, Sharma N, Kumar A: Ruptured globe 10 years after radial keratotomy. J Refract Surg 15:64, 1999 504. Vinger PF, Mieler WF, Oestreicher JH, et al: Ruptured globes following radial and hexagonal keratotomy surgery. Arch Ophthalmol 114:129, 1996 505. Zhaboedov GD, Bondareva GS: [Traumatic rupture of the eyeball after radial keratotomy]. Vestn Oftalmol 106:64, 1990 506. Wilson K, Rontal E, Rontal M: Facial injuries in football. Trans Am Acad Ophthalmol Otolaryngol 77:ORL434, 1973* 507. Rontal E, Rontal M: Maxillofacial injuries in football players: an evaluation of current facial
protection. J Sports Med Phys Fitness 11:241, 1971 508. Zemper E: Injury rates in a national sample of college football teams: a 2-year
prospective study. Phys Sportsmed 17:100, 1989 509. Sherwood DJ: Eye injuries to football players. N Engl J Med 320:742, 1989 510. Heinrichs E, Willcockson J: Catastrophic eye injury in a football player. Phys Sportsmed 10:71, 1982 511. Havkins S: Head, neck, face, and shoulder injuries in female and male rugby players. Phys Sportsmed 14:111, 1986 512. Duguid IG, Leaver PK: Giant retinal tears resulting from eye gouging in rugby football. Br J Sports Med 34:65, 2000 513. Tomasin J, Martin DF, Curl W: Recognition and prevention of rugby injuries. Phys Sportsmed 17:114, 1989 514. National Society to Prevent Blindness: Sports and recreational eye injuries. Schaumburg, IL: National Society to Prevent Blindness, 1991 515. Sime D: Personal communication; 1985 516. Jordan B, Voy R, Stone J: Amateur boxing injuries at the US Olympic training center. Phys Sportsmed 18:81, 1990 517. Hazar M, Beyleroglu M, Subasi M, et al: Ophthalmological findings in elite amateur Turkish boxers. Br J Sports Med 36:428, 2002 518. Welch M, Sitler M, Kroeten H: Boxing injuries from an instructional program. Phys Sportsmed 14:81, 1986 519. Enzenauer RW, Mauldin WM: Boxing-related ocular injuries in the United States Army, 1980 to 1985. South Med J 82:547, 1989 520. Enzenauer RW, Montrey JS, Enzenauer RJ, et al: Boxing-related injuries in the US Army, 1980 through 1985. JAMA 261:1463, 1989 521. Buttery C: Boxing in the Army. JAMA 262:2089, 1989 522. Finney J: Boxing in the Army. JAMA 262:2089, 1989 523. Jordan B. Boxing in the Army. JAMA 262:2089, 1989 524. Swartzberg D: Air Force Academy ends mandatory boxing activity. JAMA 274:784, 1995 525. Giovinazzo VJ, Yannuzzi LA, Sorenson JA, et al: The ocular complications of boxing. Ophthalmology 94:587, 1987 526. Smith DJ: Ocular injuries in boxing. Int Ophthalmol Clin 28:242, 1988 527. Smith D: Ocular injuries in boxers. Paper presented at: Science Writers' Seminar. New York: October 1986 528. Goldstein M: The incidence of ocular complications in professional boxers. American Academy of Ophthalmology, San Francisco: 1991 529. Maguire JI, Benson WE: Retinal injury and detachment in boxers. JAMA 255:2451, 1986 530. Wedrich A, Velikay M, Binder S, et al: Ocular findings in asymptomatic amateur boxers. Retina 13:114, 1993 531. Palmer E, Lieberman TW, Burns S: Contusion angle deformity in prizefighters. Arch Ophthalmol 94:225, 1976 532. Leach A, McGalliard J, Dwyer MH, et al: Ocular injuries from boxing. BMJ 304:839, 1992 533. McLeod D: Ocular injuries from boxing. BMJ 304:197, 1992 534. Vadala G, Mollo M, Roberto S, et al: Boxing and the eyes: morphological aspects of the ocular system in boxers. Eur J Ophthalmol 7:174, 1997 535. Venco L, Rigamonti L, Boschetti G: [Considerations on the ocular injuries in boxing and on a case of
detachment of the retina occurring during a fight]. Minerva Oftalmol 8:161, 1966 536. McCown I: Boxing safety and injuries. Phys Sportsmed 7:75, 1979 537. Moore M: A pall over boxing. Phys Sportsmed 11:21, 1983 538. Ludwig R: Making boxing safer: the Swedish model. JAMA 255:2482, 1986 539. Patterson RH, Jr: On boxing and liberty. JAMA 255:2481, 1986 540. Lundberg G: Boxing should be banned in civalized countries—round 3. JAMA 255:2483, 1986 541. Cantu R: Boxing and Medicine. Champaign, IL: Human Kinetics, 1995. 542. Nash H: Making boxing safer: a fight-doc's view. Phys Sportsmed 13:145, 1985 543. Enzenauer RJ: Let's stop boxing in the Olympics and the US military. JAMA 272:1821, 1994 544. Haines JD, Jr: . Let's stop boxing in the Olympics and the US military. JAMA 272:1821, 1994 545. Hage P: Boxing: to ban or not to ban? Phys Sportsmed 11:143, 1983 546. Lundberg GD: Boxing should be banned in civilized countries. JAMA 249:250, 1983 547. Ryan A: Eliminate boxing gloves. Phys Sportsmed 11:49, 1983 548. Morrison RG: Medical and public health aspects of boxing. JAMA 255:2475, 1986 549. American Academy of Ophtjalmology: Policy statement: reforms for the prevention
of eye injuries in boxing. San Francisco: Eye Safety and Sports Ophthalmology Committee, American Academy of Ophthalmology, June 23 1990 550. Powell JW: National Athletic Injury/Illness Reporting System: eye injuries in college
wrestling. Int Ophthalmol Clin 21:47, 1981 551. Paavola M: Case report. Personal Communication, Tampere, Finland; 1984 552. Putukian M, Prout B, Roberts W: A custom face mask for sports. Phys Sportsmed 28:128, 2000 553. Belongia EA, Goodman JL, Holland EJ, et al: An outbreak of herpes gladiatorum at a high-school wrestling camp. N Engl J Med 325:906, 1991 554. Holland EJ, Mahanti RL, Belongia EA, et al: Ocular involvement in an outbreak of herpes gladiatorum. Am J Ophthalmol 114:680, 1992 555. White J: Vigilance vanquishes herpes gladiatorum. Phys Sportsmed 20:56, 1992 556. Nelson M, Goldberg B: Stopping the spread of herpes simplex: a focus on wrestlers. Phys Sportsmed 20:117, 1992 557. Renneker M: Medical aspects of surfing. Phys Sportsmed 15:96, 1987 558. Gillilan R: Vision and water sports. J Am Optometric Assoc 51:683, 1980 559. Williamson DE: Correction of ametropia in skin and scuba divers. Eye Ear Nose Throat Mon 49:165, 1970 560. Malone L, Sanders R, Schlitz J, et al: Effects of visual impairment on stroke parameters in paraoplypic swimmers. Med. Sci. Sports Exerc 33:2098, 2002 561. Legerton JA: Prescribing for water sports. Optom Clin 3:91, 1993 562. Harrell WA: Lifeguards' vigilance: effects of child-adult ratio and lifeguard
positioning on scanning by lifeguards. Psychol Rep 84:193, 1999 563. Jonasson F: Swimming goggles causing severe eye injuries. Br Med J 1:881, 1977 564. Green MF, Cuthbert MF, Stebbing SJ: Swimming goggles and eye injuries. BMJ 1:1410, 1977 565. Killer HE, Blumer BK, Rust ON: Avulsion of the optic disc after a blow to swimming goggles. J Ophthalmic Nurs Technol 19:232, 2000 566. Lamb RJ: Swimming goggles causing severe eye injuries. BMJ 1:1281, 1977 567. Levy DS: Avulsion of the optic disc after a blow to swimming goggles. J Pediatr Ophthalmol Strabismus 36:111, 1999 568. Plaut GS: Diplopia in a swimmer due to badly fitting goggles. Postgrad Med J 74:607, 1998 569. Wirta DL, Dailey RA, Wobig JL: Eyelid neuroma associated with swim goggle use. Arch Ophthalmol 116:1537, 1998 570. Jordan DR, Gilberg S, Khouri L: Eyelid masses associated with competitive swimming goggles. Can J Ophthalmol 36:339, 2001 571. Ruban JM, Mallem M: [The eyelid of the competitive swimmer]. J Fr Ophtalmol 18:426, 1995 572. Pestronk A, Pestronk S: Goggle migraine. N Engl J Med 308:226, 1983 573. Joselow M: Goggles increase eye pressure. Phys Sportsmed 11:16, 1983 574. Craig A: Physics and physiology of swimming goggles. Phys Sportsmed 12:107, 1984 575. Doyle SJ: Acute corneal erosion from the use of anti-misting agent in swimming
goggles. Br J Ophthalmol 78:419, 1994 576. Stein H: Swimming with soft contact lenses. Contact Lens J 10:10, 1976 577. Stehr-Green JK, Bailey TM, Brandt FH, et al: Acanthamoeba keratitis in soft contact lens wearers. A case-control
study. JAMA 258:57, 1987 578. Barnes L: Pure pools and ponds for a safe summertime. Phys Sportsmed 6:113, 1978 579. Soni PS, Pence NA, DeLeon C, et al: Feasibility of extended wear lens use in chlorinated swimming pools. Am J Optom Physiol Opt 63:171, 1986 580. Diefenbach CB, Soni PS, Gillespie BJ, et al: Extended wear contact lens movement under swimming pool conditions. Am J Optom Physiol Opt 65:710, 1988 581. Auerbach PS: Marine envenomations. N Engl J Med 325:486, 1991 582. Glasser DB, Noell MJ, Burnett JW, et al: Ocular jellyfish stings. Ophthalmology 99:1414, 1992 583. Rapoza PA, West SK, Newland HS, et al: Ocular jellyfish stings in Chesapeake Bay watermen. Am J Ophthalmol 102:536, 1986 584. Winkel KD, Hawdon GM, Ashby K, et al: Eye injury after jellyfish sting in temperate Australia. Wilderness Environ Med 13:203, 2002 585. Alcelik T, Cekic O, Totan Y: Ocular leech infestation in a child. Am J Ophthalmol 124:110, 1997 586. Steinkuller PG, Kelly MT, Sands SJ, et al: Vibrio parahaemolyticus endophthalmitis. J Pediatr Ophthalmol Strabismus 17:150, 1980 587. Allen RH, Eiseman B, Straehley CJ, et al: Surfing injuries at Waikiki. JAMA 237:668, 1977 588. Rudolph R: Management of surfing injuries: a plastic surgeon's viewpoint. Phys Sportsmed 17:110, 1989 589. Pacelli L: Water polo's benefits surface. Phys Sportsmed 19:119, 1991 590. Melamed Y, Shupak A, Bitterman H: Medical problems associated with underwater diving. N Engl J Med. 326:30, 1992 591. Becker G: Barotrauma resulting from scuba diving: an otolaryngological perspective. Phys Sportsmed 13:113, 1985 592. Rudge FW: Ocular barotrauma caused by mask squeeze during a scuba dive. South Med J 87:749, 1994 593. Senn P, Helfenstein U, Senn ML, et al: [Ocular barostress and barotrauma. A study of 15 scuba divers]. Klin Monatsbl Augenheilkd 218:232; discussion 237, 2001 594. Mader C: [Barotrauma in diving]. Wien Med Wochenschr 151:126, 1999 595. Andenmatten R, Piguet B, Klainguti G: Orbital hemorrhage induced by barotrauma. Am J Ophthalmol 118:536, 1994 596. Merle H, Drault JN, Gerard M, et al: [Retinal vein occlusion and deep-sea diving]. J Fr Ophtalmol 20:456, 1997 597. Simon DR, Bradley ME: Corneal edema in divers wearing hard contact lenses. Am J Ophthalmol 85:462, 1978 598. Cotter J: Soft contact lens testing on fresh water scuba divers. Contact Lens 7:323, 1981 599. Isenberg SJ, Diamant A: Scuba diving after enucleation. Am J Ophthalmol 100:616, 1985 600. Lin L: Scuba divers wuth disabilities challenge medical protocols and ethics. Phys Sportsmed 15:224, 1987 601. Legwold G: Pterygium found in Olympic sailors. Phys Sportsmed 11:23, 1983 602. May JW, Jr: . The water-skier seer syndrome. N Engl J Med 300:865, 1979 603. Pearl A, Freeman J, Hurwitz J, et al: A bizarre risk of barefoot waterskiing. Phys Sportsmed 20:121, 1992 604. Cinque C: Are water bikes a water menace? Phys Sportsmed 17:31, 1989 605. Branche CM, Conn JM, Annest JL: Personal watercraft-related injuries. A growing public health concern. JAMA 278:663, 1997 606. Rogers G: Bike Helmets. Consumer Product Safety Review. 4:1, 1999 607. Schnober D, Meyer-Rusenberg HW: [Bulbar dislocation]. Klin Monatsbl Augenheilkd 199:367, 1991 608. Lessell S: Indirect optic nerve trauma. Arch Ophthalmol 107:382, 1989 609. Levin LA, Beck RW, Joseph MP, et al: The treatment of traumatic optic neuropathy: the International Optic Nerve
Trauma Study. Ophthalmology 106:1268, 1999 610. Thompson DC, Nunn ME, Thompson RS, et al: Effectiveness of bicycle safety helmets in preventing serious facial injury. JAMA 276:1974, 1996 611. Thompson DC, Rivara FP, Thompson RS: Effectiveness of bicycle safety helmets in preventing head injuries. A
case-control study. JAMA 276:1968, 1996 612. Rivara FP, Thompson DC, Thompson RS, et al: The Seattle children's bicycle helmet campaign: changes in helmet
use and head injury admissions. Pediatrics 93:567, 1994 613. Thompson RS, Rivara FP, Thompson DC: A case-control study of the effectiveness of bicycle safety helmets. N Engl J Med. 320:1361, 1989 614. Rivara FP, Thompson DC, Patterson MQ, et al: Prevention of bicycle-related injuries: helmets, education, and
legislation. Annu Rev Public Health 19:293, 1998 615. Rivara FP, Astley SJ, Clarren SK, et al: Fit of bicycle safety helmets and risk of head injuries in children. Inj Prev 5:194, 1999 616. Ching RP, Thompson DC, Thompson RS, et al: Damage to bicycle helmets involved with crashes. Accid Anal Prev 29:555, 1997 617. Thompson DC, Thompson RS, Rivara FP, et al: A case-control study of the effectiveness of bicycle safety helmets
in preventing facial injury. Am J Public Health 80:1471, 1990 618. Thompson DC, Thompson RS, Rivara FP: Incidence of bicycle-related injuries in a defined population. Am J Public Health 80:1388, 1990 619. Waller JA: The dangers of the bicycle. N Engl J Med 285:747, 1971 620. Waller JA: Bicycle ownership, use, and injury patterns among elementary school children. Pediatrics 47:1042, 1971 621. Rivara FP, Thompson DC, Thompson RS: Epidemiology of bicycle injuries and risk factors for serious injury. Inj Prev 3:110, 1997 622. Gibson M, King R: Bicycle stage racing: a model for medical support. Phys Sportsmed 20:109, 1992 623. Autzen T, Vestergaard J: [A perforation injury of the eye resulting from a car battery explosion]. Ugeskr Laeger 145:2219, 1983 624. Davidorf FH: Battery explosions: a hazard to health. JAMA 223:1509, 1973 625. Holekamp TL: Ocular injuries from automobile batteries. Trans Am Acad Ophthalmol Otolaryngol 83:805, 1977 626. Horan EC: Perforating eye injuries in Cork. A review. Trans Ophthalmol Soc UK 99:511, 1979 627. Moore AT, Cheng H, Boase DL: Eye injuries from car battery explosions. Br J Ophthalmol 66141, 1982 628. Zieker AW, Wisnicki J: Corneal burns from watch battery explosion. Am J Ophthalmol 88:798, 1979 629. Maguire L: The battery safety sticker. Sightsaving 54:12, 1985 630. Lister DG, Carl J III , Morgan JH, et al: III , Pediatric all-terrain vehicle trauma: a 5-year statewide
experience. J Pediatr Surg 33:1081, 1998 631. Margolis JL: All-terrain vehicle accidents in Maine. J Trauma 28:395, 1998 632. Reid D, Sabboe L, Allan D: Spine trauma associated with off-road vehicles. Phys Sportsmed 16:143, 1988 633. Marciani RD, Caldwell GT, Levine HJ: Maxillofacial injuries associated with all-terrain vehicles. J Oral Maxillofac Surg 57:119, 1999 634. Trammel T, Olvey S, Reed D: Championship car racing accidents and injuries. Phys Sportsmed 14:115, 1986 635. 2000 Helmet Standard For Protective Headgear for Use in Competitive Automotive
Sports. North Highlands, CA: Snell Memorial Foundation, Inc., 2000 636. Bock H: Safety measures at the Indianopolis Motor Speedway. Sports Med Bull 21:10, 1986 637. Vygantas C: Traumatic Retinal Angiopathy in Race Car Drivers. Dallas: American Academy of Ophthalmology , 1992. 638. Proscia N, Sullivan T, Cuff S, et al: The effects of motorcycle helmet use between hospitals in states with and
without a mandatory helmet law. Conn Med 66:195, 2002 639. Kraus JF, Peek C, McArthur DL, et al: The effect of the 1992 California motorcycle helmet use law on motorcycle
crash fatalities and injuries. JAMA 272:1506, 1994 640. Hotz GA, Cohn SM, Popkin C, et al: The impact of a repealed motorcycle helmet law in Miami-Dade County. J Trauma 52:469, 2002 641. Murdock MA, Waxman K: Helmet use improves outcomes after motorcycle accidents. West J Med 155370, 1991 642. Vaughan RG: Motor cycle helmets and facial injuries. Med J Aust 1:125, 1977 643. Safer eyewear for motorcyclists. ASTM Stand News 26:12, 1998 644. Nakaishi H, Yamamoto M, Ishida M, et al: Pingueculae and pterygia in motorcycle policemen. Ind Health 35:325, 1997 645. Russo PK: Easy rider—hard facts: motorcycle helmet laws. N Engl J Med 299:1074, 1978 646. Daniel RK, Midgley RD: Facial fractures in snowmobile injuries. Plast Reconstr Surg. 49:38, 1972 647. Rigg BM: Facial fractures and snowmobile accidents. Can J Surg 20:275, 1977 648. Wenzel F, Peters R: A ten-year survey of snowmobile accidents, injuries, and fatalities
in Wisconsin. Phys Sportsmed 14:140, 1986 649. Ducharme J, To KW: Exercise band-induced hyphema. Arch Ophthalmol 113:142, 1995 650. Capao Filipe JA, Pinto A, Rosas V, et al: Retinal complications after bungee jumping. Int Ophthalmol 18:359, 1995 651. Amgwerd MG: [Acute venous stasis in the area of the head after bungee-jumping. A
report of 2 cases]. Unfallchirurg 98:447, 1995 652. Chan J: Ophthalmic complications after bungee jumping. Br J Ophthalmol 78:239, 1994 653. David DB, Mears T, Quinlan MP: Ocular complications associated with bungee jumping. Br J Ophthalmol 78:234, 1994 654. Filipe JA, Pinto AM, Rosas V, et al: Retinal complications after bungee jumping. Int Ophthalmol 18:359, 1994 655. Habib NE, Malik TY: Visual loss from bungee jumping. Lancet 343:487, 1994 656. Innocenti E, Bell TA: Ocular injury resulting from bungee-cord jumping. Eye 8(Pt 6):710, 1994 657. Jain BK, Talbot EM: Bungee jumping and intraocular haemorrhage. Br J Ophthalmol 78:236, 1994 658. Simons R, Krol J: Visual loss from bungee jumping. WLancet 343:853, 1994 659. Van Rens E: Traumatic ocular haemorrhage related to bungee jumping. Br J Ophthalmol 78:948, 1994 660. Krott R, Mietz H, Krieglstein GK: Orbital emphysema as a complication of bungee jumping. Med Sci Sports Exerc 29:850, 1997 661. Worthen DM: Retinal detachment and jogging. Ophthalmic Surg 11:253, 1980 662. Bovino JA, Marcus DF: Physical activity after retinal detachment surgery. Am J Ophthalmol 98:171, 1984 663. Itin P, Haenel A, Stalder H: From the heavens, revenge on joggers. N Engl J Med 311:1703, 1984 664. Eisner T: Still more on bird attacks. N Engl J Med 313:1232, 1985 665. Kobet KA: Retinal tear associated with gravity boot use. Ann Ophthalmol 17:308, 1985 666. Klatz RM, Goldman RM, Pinchuk BG, et al: The effects of gravity inversion procedures on systemic blood pressure, intraocular
pressure, and central retinal arterial pressure. J Am Osteopath Assoc 82:853, 1983 667. Moses RA, Grodzki WJ, Jr: . Mechanism of glaucoma secondary to increased venous pressure. Arch Ophthalmol 103:1701, 1985 668. Friberg TR, Sanborn G, Weinreb RN: Intraocular and episcleral venous pressure increase during inverted posture. Am J Ophthalmol 103:523, 1987 669. Weinreb RN, Cook J, Friberg TR: Effect of inverted body position on intraocular pressure. Am J Ophthalmol 98:784, 1984 670. Friberg TR, Sanborn G: Optic nerve dysfunction during gravity inversion. Pattern reversal visual
evoked potentials. Arch Ophthalmol 103:1687, 1985 671. Sanborn GE, Friberg TR, Allen R: Optic nerve dysfunction during gravity inversion. Visual field abnormalities. Arch Ophthalmol 105:774, 1987 672. Rice R, Allen RC: Yoga in glaucoma. Am J Ophthalmol . Nov 15 1985;100(5):738–739 673. Gungor K, Beydagi H, Bekir N, et al: The impact of acute dynamic exercise on intraocular pressure: role of the
beta 2-adrenergic receptor polymorphism. J Int Med Res 30:26, 2002 674. Passo MS, Goldberg L, Elliot DL, et al: Exercise training reduces intraocular pressure among subjects suspected
of having glaucoma. Arch Ophthalmol 109:1096, 1991 675. Qureshi IA: Effects of mild, moderate and severe exercise on intraocular pressure of
sedentary subjects. Ann Hum Biol 22:545, 1995 676. Qureshi IA: The effects of mild, moderate, and severe exercise on intraocular pressure
in glaucoma patients. Jpn J Physiol 45:561, 1995 677. Qureshi IA: Effects of exercise on intraocular pressure in physically fit subjects. Clin Exp Pharmacol Physiol 23:648, 1996 678. Qureshi IA: Does physical fitness influence intraocular pressure? J Pak Med Assoc 47:81, 1997 679. Kypke W, Hermannspann U: [Glaucoma physical activity and sport (author's transl)]. Klin Monatsbl Augenheilkd 164:321, 1974 680. Stewart RH, LeBlanc R, Becker B: Effects of exercise on aqueous dynamics. Am J Ophthalmol 69:245, 1970 681. Shah P, Whittaker KW, Wells AP, et al: Exercise-induced visual loss associated with advanced glaucoma in
young adults. Eye 15(Pt 5):616, 2001 682. Epstein DL, Boger WP III , Grant WM: Phenylephrine provocative testing in the pigmentary dispersion syndrome. Am J Ophthalmol 85:43, 1978 683. Haynes WL, Johnson AT, Alward WL: Effects of jogging exercise on patients with the pigmentary dispersion
syndrome and pigmentary glaucoma. Ophthalmology 99:1096, 1992 684. Jensen PK, Nissen O, Kessing SV: Exercise and reversed pupillary block in pigmentary glaucoma. Am J Ophthalmol 120:110, 1995 685. Doyle WJ, Weber PA, Meeks RH: Effect of topical timolol maleate on exercise performance. Arch Ophthalmol 102:1517, 1984 686. Atkins JM, Pugh BR, Jr: , Timewell RM: Cardiovascular effects of topical beta-blockers during exercise. Am J Ophthalmol 99:173, 1985 687. Carswell H: Headaches: a weighty problem for lifters? Phys Sportsmed 12:23 1984 688. Rennie D, Morrissey J: Retinal changes in Himalayan climbers. Arch Ophthalmol 93:395, 1975 689. Shults WT, Swan KC: High altitude retinopathy in mountain climbers. Arch Ophthalmol 93:404, 1975 690. Wiedman M: High altitude retinal hemorrhage. Arch Ophthalmol 93:401, 1975 691. Butler FK, Harris DJ Jr. , Reynolds RD: Altitude retinopathy on Mount Everest, 1989. Ophthalmology 99:739, 1992 692. Wiedman M, Tabin GC: High-altitude retinopathy and altitude illness. Ophthalmology 106:1924; discussion 1927, 1992 693. Lang GE, Kuba GB: High-altitude retinopathy. Am J Ophthalmol 123418, 1997 694. Koch DD, Knauer WJ, III , Emery JM: High altitude corneal endothelial decompensation. Cornea 3:189, 1984 695. Hanscom TA, Diddie KR: Mountain travel and intraocular gas bubbles. Am J Ophthalmol 104:546, 1987 696. Mills MD, Devenyi RG, Lam WC, et al: An assessment of intraocular pressure rise in patients with gas-filled
eyes during simulated air flight. Ophthalmology 108:40, 2001 697. Wilkerson J: Medicine for Mountaineering. Seattle: Mountaineers, 1967 698. DeBenedette V: Sunglasses for mountaineers: personal experience shared. Ophthalmology Times September 1:31, 1983 699. Mader TH, White LJ, Johnson DS, et al: The ascent of Mount Everest following radial keratotomy. Wilderness Environ Med 13:53, 2002 700. Winkle RK, Mader TH, Parmley VC, et al: The etiology of refractive changes at high altitude after radial keratotomy. Hypoxia
versus hypobaria. Ophthalmology 105:282, 1998 701. Creel DJ, Crandall AS, Swartz M: Hyperopic shift induced by high altitude after radial keratotomy. J Refract Surg 13:398, 1997 702. Mader TH, Blanton CL, Gilbert BN, et al: Refractive changes during 72-hour exposure to high altitude after
refractive surgery. Ophthalmology 103:1188, 1996 703. Ng JD, White LJ, Parmley VC, et al: Effects of simulated high altitude on patients who have had radial keratotomy. Ophthalmology 103:452, 1996 704. Mader TH, White LJ: Refractive changes at extreme altitude after radial keratotomy. Am J Ophthalmol 119:733, 1995 705. Boes DA, Omura AK, Hennessy MJ: Effect of high-altitude exposure on myopic laser in situ keratomileusis. J Cataract Refract Surg 27:1937, 2001 706. Dimmig JW, Tabin G: The ascent of Mount Everest following laser in situ keratomileusis. J Refract Surg 19:48, 2003 707. DeBenedette V: People and horses: the risks of riding. Phys Sportsmed 17:251–254, 1989 708. Bixby-Hammett D: Youth accidents with horses. Phys Sportsmed :105, 1985 709. Brooks W, Bixby-Hammett D: Prevention of neurologic injuries in equestrian sports. Phys Sportsmed 16:84, 1988 710. Bixby-Hammett D: Head injuries in the equestrian sports. Phys Sportsmed 11:82, 1983 711. Nelson D, Rivara F, Condie C, et al: Injuries in equestrian sports. Phys Sportsmed 22:53, 1994 712. Waller AE, Daniels JL, Weaver NL, et al: Jockey injuries in the United States. JAMA 283:1326, 2000 713. Malavase D: Promoting the use of F1163. ASTM Stand News November:2, 1991 714. US Pony Club Accident Study: Facial and Eye Injuries. Lexington, KY, 1992. 715. Bixby-Hammett D: United States Pony Club Accident Study 1982–1992. Lexington, KY, 1993 716. Butterwick DJ, Hagel B, Nelson DS, et al: Epidemiologic analysis of injury in five years of Canadian professional
rodeo. Am J Sports Med 30:193, 2002 717. Ketai LH, Temes RT, Deis JL, et al: Rodeo related large animal injury: is protective head-gear warranted? Injury 31:757, 2000 718. Griffin R, Peterson K, Halseth J, et al: Injuries in profssional rodeo: an update. Phys Sportsmed 15:105, 1987 719. Griffin R, Peterson K, Halseth J: Injuries in professional rodeo. Phys Sportsmed 11:110, 1983 720. Eichler J: [Eye accidents due to ski-pole injuries]. Dtsch Gesundheitsw 27:375, 1972 721. Morrow P: Downhill ski fatalities: the Vermont experience. Boston: National Association of Medical Examiners, 1988 722. Brown J: Snow sports: down the tube. Phys Sportsmed: 152–154, 1979 723. CPSC. Fact sheet: sleds, toboggans, and snow discs. Washington, DC: US Consumer Product Safety Commission, 1974 724. Roos R: Luge participation is hard on the head. Phys Sportsmed 14:185, 1986 725. Jackson RW, Fredrickson A: Sports for the physically disabled. The 1976 Olympiad (Toronto). Am J Sports Med 7:293, 1979 726. Malpass JJ: USABA national championships—a sight to behold. J Am Optom Assoc 51:693, 1980 727. Ross J: Blind break theough old barriers to sports. Phys Sportsmed March :98, 1977 728. Sherrill C, Hinson M, Gench B, et al: Self-concepts of disabled youth athletes. Percept Mot Skills 70(3 Pt 2):1093, 1990 729. Talmachev RA: [Present-day sports activities among the blind and persons
with poor vision in different countries of the world]. Vestn Oftalmol 119:43, 2003 730. Reynolds J, Stirk A, Thomas A, et al: Paralympics—Barcelona 1992. Br J Sports Med 28:14, 1994 731. Makris VI, Yee RD, Langefeld CD, et al: Visual loss and performance in blind athletes. Med Sci Sports Exerc 25:265, 1993 732. Ferrara MS, Buckley WE, Messner DG, et al: The injury experience and training history of the competitive skier with
a disability. Am J Sports Med 20:55, 1992 733. Watts R, Bahill A: Keep Your Eye On the Ball: The Science and Folklore of Baseball. New York: Freeman & Company, 1990. 734. Laby DM, Rosenbaum AL, Kirschen DG, et al: The visual function of professional baseball players. Am J Ophthalmol 122:476, 1996 735. Seiderman A, Schneider S: The Athletic Eye: Improved Sports Performance Through Visual Training. New York: Hearst Books, 1983 736. Druckman D, Swets J: Enhancing Human Performance: Issues, Theories, and Techniques. Washington, DC: National Academy Press, 1988 737. Vickers JN: Visual control when aiming at a far target. J Exp Psychol Hum Percept Perform 22:342, 1996 738. Vickers JN: Gaze control in putting. Perception 21:117, 1992 739. Oudejans RR, van de Langenberg RW, Hutter RI: Aiming at a far target under different viewing conditions: visual control
in basketball jump shooting. Hum Mov Sci 21:457, 2002 740. Shaffer DM, McBeath MK: Baseball outfielders maintain a linear optical trajectory when tracking
uncatchable fly balls. J Exp Psychol Hum Percept Perform 28:335, 2002 741. Moreno FJ, Reina R, Luis V, et al: Visual search strategies in experienced and inexperienced gymnastic coaches. Percept Mot Skills 95(3 Pt 1):901, 2002 742. Reed CL: Chronometric comparisons of imagery to action: visualizing versus physically
performing springboard dives. Mem Cognit 30:1169, 2002 743. Williams AM, Ward P, Knowles JM, et al: Anticipation skill in a real-world task: measurement, training, and
transfer in tennis. J Exp Psychol Appl 8:259, 2002 744. Al-Abood SA, Bennett SJ, Hernandez FM, et al: Effect of verbal instructions and image size on visual search strategies
in basketball free throw shooting. J Sports Sci 20:271, 2002 745. Rodrigues ST, Vickers JN, Williams AM: Head, eye and arm coordination in table tennis. J Sports Sci 20:187, 2002 746. Savelsbergh GJ, Williams AM, Van der Kamp J, et al: Visual search, anticipation and expertise in soccer goalkeepers. J Sports Sci 20:279, 2002 747. Gray R: Behavior of college baseball players in a virtual batting task. J Exp Psychol Hum Percept Perform 28:1131, 2002 748. Rotberg MH: Biofeedback for ophthalmologic disorders. Surv Ophthalmol 27:381, 1983 749. Trachtman JN: Biofeedback of accommodation to reduce myopia: a review. Am J Optom Physiol Opt 64:639, 1987 750. Koslowe KC, Spierer A, Rosner M, et al: Evaluation of accommotrac biofeedback training for myopia control. Optom Vis Sci 68:338, 1991 751. Classe JG: Legal aspects of sports vision. Optom Clin 3:27, 1993 752. Classe JG: Legal aspects of sports-related ocular injuries. Int Ophthalmol Clin 28:211, 1988 753. Classe JG, Scholles J: Liability for ophthalmic materials. J Am Optom Assoc 57:470, 1986 754. Editorial. NOCSAE: Another victim of liability crisis. Athletic Business June:33, 1987 755. Lubell A: Insurance, liability, and the American way of sport. Phys Sportsmed 15:192, 1987 756. Editorial. Risk management is the best insurance. Athletic Business June:36, 1987 757. Bettman JW, Tennenhouse DJ: Some legal decisions significant for ophthalmology. Surv Ophthalmol 32:32, 1987 758. Kraushar MF, Robb JH: Ophthalmic malpractice lawsuits with large monetary awards. Arch Ophthalmol 114:333, 1996 759. Adams S, Bayless M: How the Seattle decision affects liability and you. Athletic Purchasing Facilities July:12, 1982 760. Editorial. Youth sports injuries; is the risk acceptable? Athletic Purchasing Facilities January:14, 1984 761. Hinson DB: Ocular sports injuries. Legal aspects. II. Lawyer's perspective. Int Ophthalmol Clin 21:209, 1981 762. McKeag D, Brody H, Hough D: Medical ethica ion sports. Phys Sportsmed 4:145, 1984 763. Corbin C: A Textbook of Motor Development. Dubuque, IA: William C. Brown, 1980 764. Hirsch E, Vaughn B: Three college sports support twenty-five varsity programs. Athletic Purchasing Facilities April/May:12, 1977 765. Murray T: Divided loyalties in sports medicine. Phys Sportsmed 12:134, 1984 766. Finkelstein D, Smith MK, Faden R: Informed consent and medical ethics. Arch Ophthalmol 111:324, 1993 767. Thompson DF: Understanding financial conflicts of interest. N Engl J Med 329:573, 1993 768. Pellegrino ED: Ethics. JAMA 270:202, 1993 769. Bullock JD, Warwar RE, Green WR: Ocular explosions from periocular anesthetic injections: a clinical, histopathologic, experimental, and biophysical study. Ophthalmologym 106:2341; discussion 2352, 1999 770. Green RP, Jr. , Peters DR, Shore JW, et al: Force necessary to fracture the orbital floor. Ophthal Plast Reconstr Surg 6:211, 1990 771. Acheson JF, Griffiths MF, Cooling RJ: Serious eye injuries due to war games. BMJ 298:26, 1989 772. Anders N: [Eye injuries caused by Gotcha games]. Klin Monatsbl Augenheilkd 204:542, 1994 773. Dawidek GMB: Serious eye injuries due to war games. BMJ 298:383, 1989 774. Easterbrook M, Pashby TJL: Eye injuries associated with war games. CMAJ 133:415, 1985 775. Farr AK, Fekrat S: Eye injuries associated with paintball guns. Int Ophthalmol 22:169–, 1998 776. Fineman MS, Fischer DH, Jeffers JB, et al: Changing trends in paintball sport-related ocular injuries. Arch Ophthalmol 118:60, 2000 777. Gazagne C, Larricart P, Haut J: [The danger of the game called “paint ball”]. Bull Acad Natl Med 178:671; discussion 677, 1994 778. Hargrave S, Weakley D, Wilson C: Complications of ocular paintball injuries in children. J Pediatr Ophthalmol Strabismus 37:338, 2000 779. Hansen MK: [Eye injuries during paintball games. The first Danish case with a
summary of foreign experiences]. Ugeskr Laeger 156:6550, 1994 780. Karel I, Pitrova S, Lest'ak J, et al: [Eye injury from a paintball projectile]. Cesk Slov Oftalmol 58:171, 2002 781. Kruger LP, Acton JK: Paintball ocular injuries. S Afr Med J 89:265, 1999 782. Mamalis N, Monson MC, Farnsworth ST, et al: Blunt ocular trauma secondary to “war games.” Ann Ophthalmol 22:416, 1990 783. Martin PL, Magolan JJ, Jr .:Eye injury during “war games” despite the use of goggles. Case
report. Arch Ophthalmol 105:321, 1987 784. Mason JO, III , Feist RM, White MF, Jr .:Ocular trauma from paintball-pellet war games. South Med J 95:218, 2002 785. Morgan SJ: Serious eye injuries due to war games. BMJ 298:383, 1989 786. Pakoulas C, Shar S, Frangoulis MA: Serious eye injuries due to war games. BMJ 298:383, 1989 787. Ryan EH, Jr. , , Lissner G: Eye injuries during ‘war games’. Arch Ophthalmol 104:1435, 1986 788. Schwartz S, Mandava N, Stout J, et al: Ocular injuries sustained during paintball: a recreational war game. Macula and Retina Society Member Survey , 2000 789. Tardif D, Little J, Mercier M, et al: Ocular trauma in war games. Phys Sportsmed 14:91, 1986 790. Thach AB, Ward TP, Hollifield RD, et al: Ocular injuries from paintball pellets. Ophthalmology 106:533, 1999 791. Verburg-van der Marel EH, ten Napel JA, de Keizer RJ: [Eye injuries in ‘paintball’; a modern ‘war injury’]. Ned Tijdschr Geneeskd 137:825, 1993 792. Wellington DP, Johnstone MA, Hopkins RJ: Bull's-eye corneal lesion resulting from war game injury. Arch Ophthalmol 107:1727, 1989 793. Welsh NH, Howes F, Lever J: Eye injuries associated with ‘war games’. S Afr Med J 76:270, 1989 794. Wrenn KD, White SJ: Injury potential in “paintball” combat simulation games: a
report of two cases. Am J Emerg Med 9:402, 1991 795. Zwaan J, Bybee L, Casey P: Eye injuries during training exercises with paint balls. Mil Med 161:720, 1996 796. Moore M, Worthley D: Ocular injury in squash players. Austr J Ophthalmol 5:46, 1977 797. Easterbrook M: Eye injuries in squash: a preventable disease. Can Med Assoc J 118:298, 1978 798. Blonstein JL: Eye injuries in sport: with particular reference to squash rackets and
badminton. Practitioner 215:208, 1975 799. Easterbrook M: Eye injuries in racket sports: a continuing problem. Phys Sportsmed 9:91, 1981 800. Easterbrook M: Eye protection for squash and racquetball players. Phys Sportsmed 9:79, 1981 801. Mondon H, Lefrancois A, Lai C, et al: [Ocular injuries in squash]. Bull Soc Ophtalmol Fr 81:303, 1981 802. Bankes J: Squash rackets: a survey of eye injuries in England. BMJ 291:1539, 1985 803. Kahle G, Dach T, Wollensak J: [Eye injuries in squash]. Klin Monatsbl Augenheilkd 203:195, 1993 804. Capao Filipe JA: Soccer (Football) Ocular Injuries: An Important Eye Health Problem. Br J. Ophthalmol 88(2):159–60 2004 805. Vinger PF, Capao Filipe JA: The Mechanism and Prevention of Soccer Eye Injuries. Br J. Ophthalmol 88(2):167–8, 2004 |