INDICATIONS AND TIMING
The indication for probing and irrigation of the lacrimal collecting system is persistent obstruction with tearing and discharge dating from the early months of the first year. Probing primarily is the initial procedure to consider for such obstruction. Except for the lacrimal puncta, the drainage system cannot be visualized directly, and probing helps to locate the level and nature of the obstruction. Fortunately, in children the probing also is highly effective in relieving the blockage,1–3 and in most instances, further procedures are not necessary.
Congenital nasolacrimal duct obstruction has a high rate of spontaneous resolution during the first year,4–7 There is some difference of opinion about how early to resort to probing to clear persistent obstructions. Early probing may clear the symptoms faster, but a routine of early probing leads to performing many procedures that would be unnecessary. I usually advise delay of probing until near the end of the first year. Mucopurulent discharge from infection in the collecting system usually is present to some degree. It can be managed with lid hygiene and the application of antibiotic ointments. Pressure over the lacrimal sac can be used to prevent accumulation of discharge. This pressure usually results in retrograde flow of the sac contents onto the eye, where they can be wiped away. Occasionally, the pressure is transmitted hydrostatically down the nasolacrimal duct, and with a sudden popping sensation the obstruction may be relieved.8 Failing this, persistent purulent discharge and lid irritation are reasons to proceed with probing. An episode of frank dacryocystitis with swelling and redness in the area of the lacrimal sac is a more pressing indication for probing. The dacryocystitis is first treated with systemic antibiotics, but subsequent probing to relieve the obstruction is necessary to prevent recurrence. A further indication to probe on an accelerated timetable is the need to clear the lacrimal system infection before anticipated ocular, facial, or intracranial surgery. Occasionally, the timing of a probe may be influenced by the need for general anesthesia for some unrelated surgery and the convenience of doing both procedures under one anesthesia.
A special indication for early probing is distention of the lacrimal sac at birth, caused by a combination of nasolacrimal duct obstruction and a physiologic canalicular blockage of retrograde flow, the so-called congenital dacryocystocele. Probing should be undertaken in the newborn period rather than later because secondary infection is likely to develop in the closed system.4,9 Beyond this, dacryocystoceles also may be associated with distention of the nasolacrimal duct and intranasal cysts, which cause respiratory distress in young infants.10,11 The lacrimal puncta and canaliculi are small at this early age, but even without anesthesia, the inferior canaliculus usually can be dilated and probed to decompress the lacrimal sac, and the distal duct obstruction can be broken by passing the probe on into the nose. Sometimes, an intranasal cyst requires a more extensive procedure, including marsupialization of the cyst with fiberoptic nasal endoscopy.11
Finally, the timing of probing and irrigation may be affected by the decision whether to perform the procedure under anesthesia. In the newborn period, the procedure usually is done without anesthesia, and many ophthalmologists prefer to perform the probe in the office with topical anesthesia until the infant is 6 months of age.1,12 Beyond 6 months, I routinely use general anesthesia in an ambulatory operating room setting.13 Probings done under general anesthesia are more comfortable for the patient, and they are technically easier and better controlled for the surgeon. An endotracheal tube usually is not required for standard probing, although without a tube, irrigation must be limited to prevent aspiration. With mask anesthesia, access to the nose is limited. A skilled pediatric anesthesia staff helps to make probing under general anesthesia a safe and reliable procedure.
CONTRAINDICATIONS
Whereas there are no absolute contraindications to probing and irrigation for persistent obstruction of the lacrimal drainage system, several considerations may affect the timing of the probe. There is no reason to perform a probe in the early months of the first year if the lacrimal sac is not distended and symptoms are manageable. Spontaneous clearing occurs in most obstructions up to at least 12 months of age.4–7 If parents are anxious about a surgical procedure, especially one under general anesthesia, additional time can be allowed for clearing. Probing should be delayed if there is an upper respiratory tract infection or if there is acute dacryocystitis. Any contraindications to general anesthesia, such as severe congenital heart disease, may delay treatment. If probing is done in the presence of congenital heart disease, prophylactic antibiotics are advisable because of the possibility of transient bacteremia.14
PROCEDURE
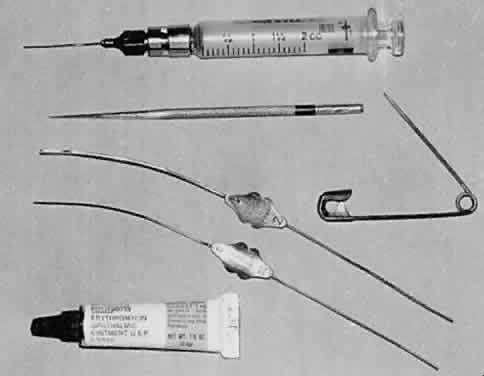
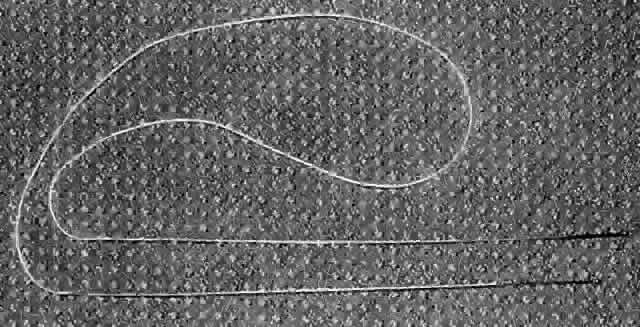
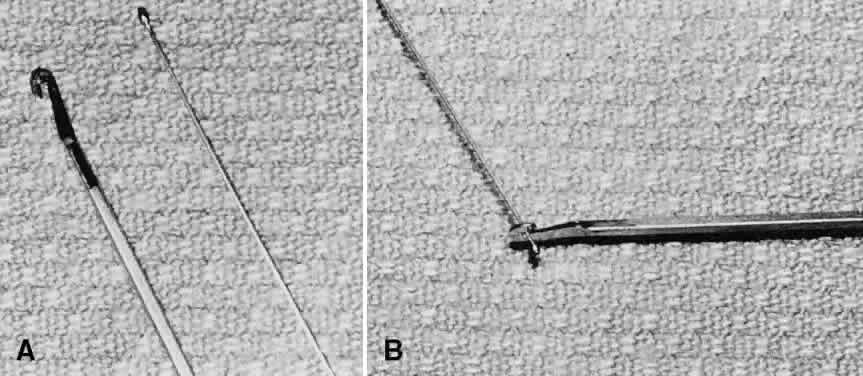
When performing a probe without anesthesia, the lower canaliculus usually is easier to enter, but under general anesthesia the upper canaliculus is the preferred access to the system. The upper punctum is dilated, and a Bowman no. 0 (0.7-mm diameter) or no. 1 (0.8-mm diameter) probe (Fig. 1) is passed through the canaliculus into the lacrimal sac (Fig. 2). Occasionally, the obstruction is at the level of the punctum itself, a blockage signaled by symptoms of tearing without discharge, and when the punctum is opened, tear flow is normalized. More often, the obstruction is at the lower end of the lacrimal duct, and the probe can be passed to that point relatively freely. It is helpful to bend the probe to a gentle curve so that after it reaches a firm stop at the medial wall of the sac in the lacrimal fossa, it can be directed down and posteriorly into the duct (Fig. 3). Lubricating the probe with an ophthalmic ointment also eases its passage. At the lower end of the lacrimal duct, slightly firmer pressure is necessary to break through the membranous obstruction into the nose. It may help to direct the curve of the probe posteriorly and medially to break into the nose under the inferior turbinate. Then the probe either stops at the floor of the nasal cavity or runs posteriorly along the surface of the hard palate. If uncertainty exists as to whether the probe has entered the nasal cavity, a second Bowman probe can be placed in the nose under the inferior turbinate to feel the contact of metal on metal. The probe then is withdrawn, and saline is irrigated through the system using a glass syringe and a 23-gauge cannula threaded through one canaliculus into the sac (Fig. 4). The other canaliculus is plugged with a lacrimal dilator to prevent reflux. Only a small amount of fluid (approximately 1 ml) is required to establish that the lacrimal duct is open; larger amounts increase the risk of aspiration. Fluorescein can be used to stain the irrigant so that it can be visualized using a clear suction catheter in the nose, but patency of the system usually can be recognized by the feel of the freely moving plunger of the glass syringe.
|
Recently, a nasolacrimal duct probe with a balloon catheter has become available as an adjunct to standard probing.15 Several reports of its use have been published,16,17 but it is not clear whether or in which cases this new instrumentation will be advantageous.
EXPECTED RESULTS
After a successful probing, tearing and discharge usually clear within 1 to 2 days. A topical antibiotic ointment or solution can be used if there is much mucopurulent discharge at the time of probing, but these are discontinued as soon as the eye appears to be clear. The normal passage of tears through the lacrimal drainage system helps to clear residual discharge. Initial probings are successful in over 90% of patients.13,12 Some surgeons have found a decrease in the success rate if the probing is delayed beyond the second or third year,18 but many patients can be cured by probing up to 5 years of age or older.2,3,19 If tearing and discharge persist after apparently successful probing, a second probing can be done in a month with the option of placing silicone tubing in the lacrimal system at that time. If it has not been possible to pass the probe into the nose because of bony obstruction at the lower end of the lacrimal duct, dacryocystorhinostomy is required to establish satisfactory tear drainage. Occasionally, the probe seems to pass into the nose, but irrigation is not free. In this case, it is unlikely that the probing will be successful. Repeat probing at the time, or reprobing with the option of silicone intubation after a 1-month interval, may resolve the issue.
COMPLICATIONS
Most probings are free of complications. A false passage of the probe may be signaled by extravasation of saline into surrounding tissues at the time of irrigation. This usually subsides in a short time, but prophylactic systemic antibiotics are advisable. Postoperative fever occasionally occurs after an otherwise unremarkable probe and probably is secondary to bacteremia induced by the probing.20 The fever subsides with antipyretics, and antibiotics are not routinely required.