MYOTOMY
An inferior oblique myotomy usually is performed between the nerve to the inferior oblique muscle and the insertion of the muscle. After the muscle is crushed with one or two hemostats, transverse surgical sectioning of the muscle is performed. Suture ligatures or cautery may be used for hemostasis. If the inferior oblique muscle is isolated properly, this procedure is not complicated and is performed rapidly. The severed ends of the inferior oblique muscle tend to reunite, however, and the preoperative state may be resumed within several months.2,10
MYECTOMY
An inferior oblique myectomy includes removal of a section of the muscle to reduce the tendency of the myotomized ends to reunite. Two hemostats are used, as with the myotomy, except that a space of 5 mm or more is maintained between the hemostats, so that the segment of muscle between the hemostats can be removed. Cautery, ligature, or both are used for hemostasis. This procedure offers the same advantages as the myectomy but the cut ends still tend to reunite.10 Parks2,11 performed a controlled prospective study comparing the various methods of weakening the inferior oblique muscle. The study included 638 consecutive patients who had a minimum follow-up of 2 years. Parks performed 19 myectomies at the origin of the inferior oblique, 86 myectomies at the insertion, 89 disinsertions, and 444 recessions of inferior oblique muscles. The overaction of the inferior oblique muscle returned in 79% of the 19 eyes that underwent a myectomy at the origin. Because the recurrence rate is high and the procedure is difficult to perform, this procedure is no longer performed. Myectomy at the insertion produced a 37% return on overaction, also causing that procedure to be abandoned by Parks. Many authors, however, still prefer this procedure and advocate its use. Dyer1 reported a 91% success rate in reducing the hypertropia to 10 diopters or less, and Davis and coworkers12 reported a 93% success rate.
DISINSERTION
Disinsertion occurs at the scleral attachment of the inferior oblique muscle. Assuming proper exposure of the inferior oblique, this procedure is performed rapidly. The reattachment rate of the inferior oblique tendon is not predictable, however. It has a tendency to attach at or near the original insertion site or to the inferior border of the lateral rectus muscle.10 Parks2,11 found a 53% rate of return of overaction, worse than that for the myectomy procedure at the insertion end. Jones and associates,13 however, reported a success rate of 88% with inferior oblique disinsertion.
RECESSION
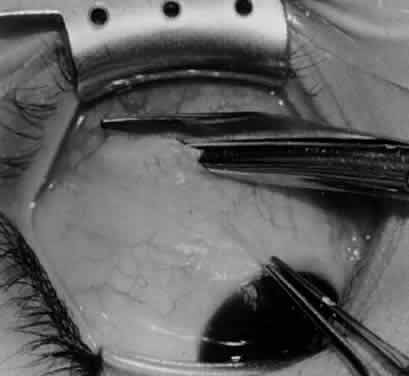
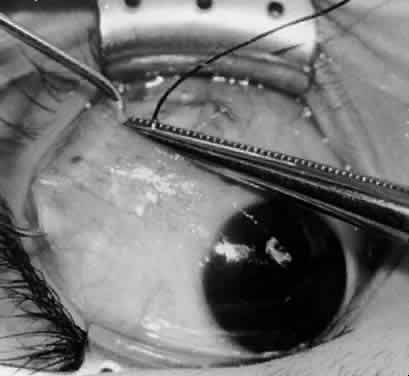
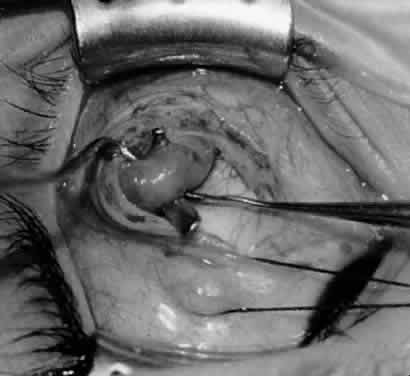
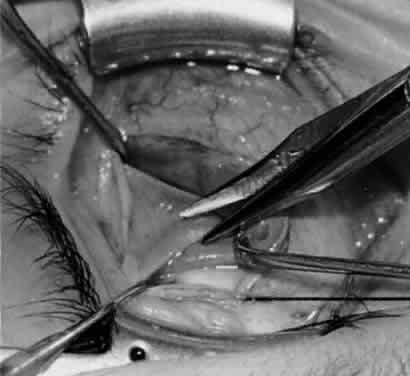
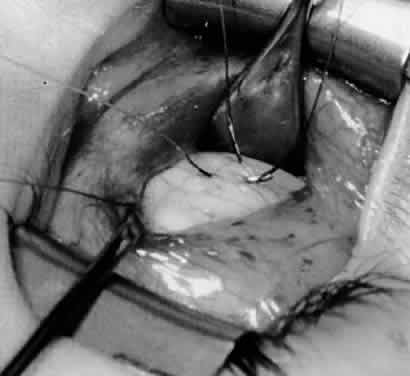
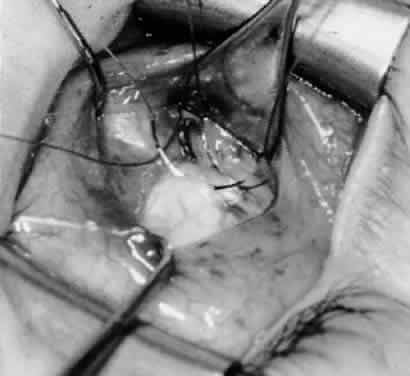
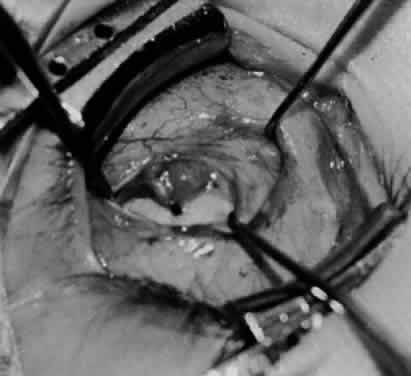
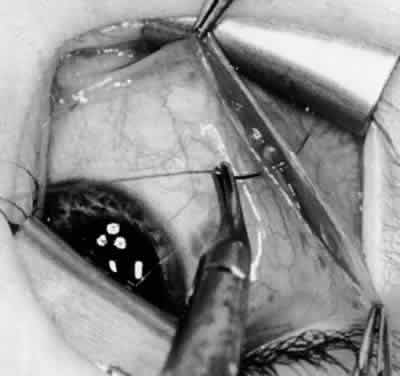
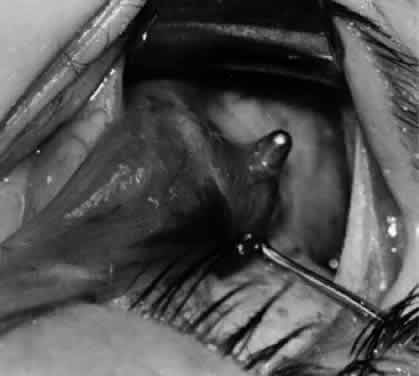
In comparing the various weakening procedures, Parks2,11 concluded that the recession procedure was superior (Figs. 1–20). The major advantage of the recession is that it allows the weakening procedure to be titrated according to the severity of the overaction. For 1+ overaction, the inferior oblique muscle is recessed 6 mm; for 2+ overaction, 10 mm; and for 3+ overaction, 14 mm, which is the maximum recession. A double-armed 6-0 synthetic suture, such as polyglactin (Vicryl [J-562]*) with a half-circle spatula needle (S-28*), is placed within the insertion of the inferior oblique with a locked bite at the anterior and posterior border (see Fig. 11). With an Aebli scissor, the muscle is sectioned from the globe (see Fig. 12) and recessed 6 mm by placing the anterior suture 4 mm lateral to the lateral insertion of the inferior rectus muscle and the posterior suture 3 mm more laterally. The 10-mm recession (see Figs. 15, 17, 18, 20) requires placement of the anterior suture 2 mm temporal and 3 mm posterior to the temporal insertion of the inferior rectus muscle, with the posterior suture placed 3 mm more posteriorly. The 14-mm recession (see Figs. 14, 16, 19, 20) requires placement of the anterior and posterior sutures parallel to the inferior-temporal vortex vein, which usually is found 8 mm posterior to the temporal insertion of the inferior rectus muscle.
|
|
|
|
|
|
|
|
|
|
|
Ethicon, Somerville, NJ.
Ethicon, Somerville, NJ.
Because the inferior oblique muscle inserts near the macula, there may be concern about penetration of the macula with a preplaced suture, which can cause macula hemorrhage, visual impairment, or visual loss. An alternative is to place a hemostat near the insertion of the inferior oblique muscle and then section the muscle from the globe with the Aebli scissor. The 6-0 Vicryl suture can be placed within the muscle, which is grasped by the hemostat and a locked bite placed at the anterior and posterior borders of the muscle, before the muscle is reattached to the sclera at the intended position. The technique of removing the inferior oblique muscle with the hemostat is part of the denervation and extirpation procedure.
The disadvantage of the recession procedure is the difficulty involved in performing the procedure within a small operative field with limited visibility, compared with the myectomy or disinsertion. With proper illumination, however, such as the surgeon wearing the operating headlight and exposure with the Desmarres or Conway lid retractor, the inferior oblique insertion readily can be seen for placement of sutures and separation of the inferior oblique from the sclera.
Parks2,11 found that 15% of patients had a return of overaction with the recession procedure, compared with 79% with myectomy at the origin, 53% with disinsertion, and 37% with myectomy at the insertion. Short-term follow-up is not helpful with oblique muscle surgery because inferior oblique overaction can return gradually over 2 years.10 Therefore, long-term follow-up is necessary for proper evaluation of success. In a more recent report, Wilson and Parks14 found a 25% recurrence rate of inferior oblique overaction after surgery, with an average follow-up of 3 years. Only 6% of patients required repeat inferior oblique surgery, however.
DENERVATION
Gonzalez15 first described denervation of the inferior oblique muscle as a weakening procedure but also reported the return of overaction within the first postoperative year.16,17 The nerve to the inferior oblique is attached tightly to the posterior belly of the inferior oblique muscle, lateral to the inferior rectus muscle border. At this site is a fusiform enlargement of the belly. After the nerve is hooked posteriorly with a Stevens hook, cautery is used to sever the nerve and the accompanying artery and vein. The procedure of denervation is no longer used alone because of the likelihood of recurrence of the inferior oblique overaction but it is used as the foundation for the denervation and extirpation procedure.
DENERVATION AND EXTIRPATION
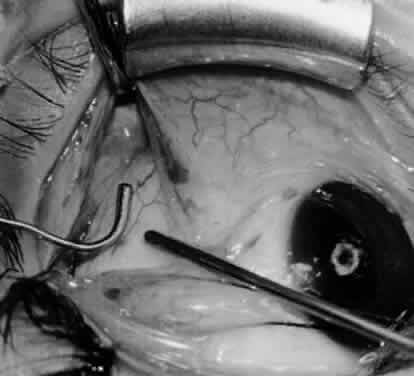
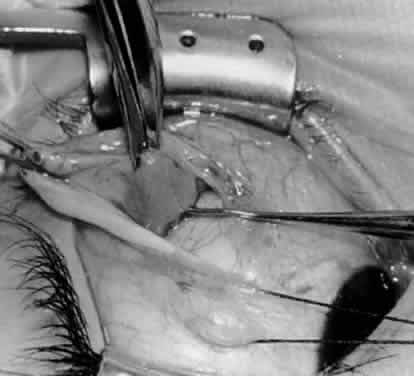
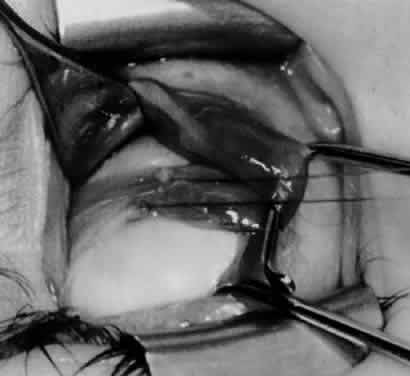
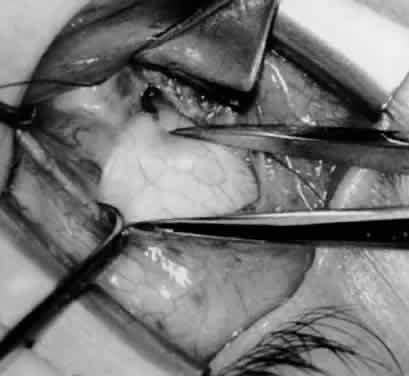
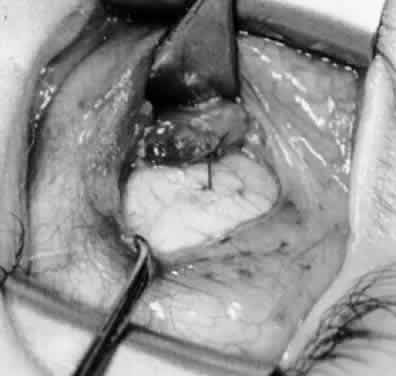
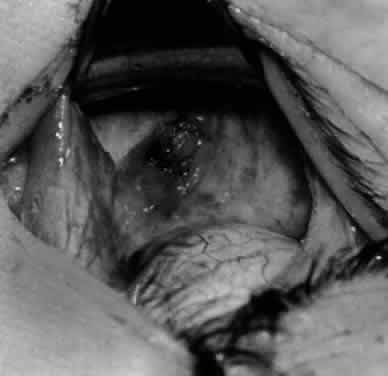
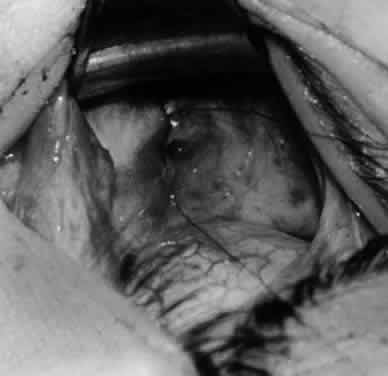
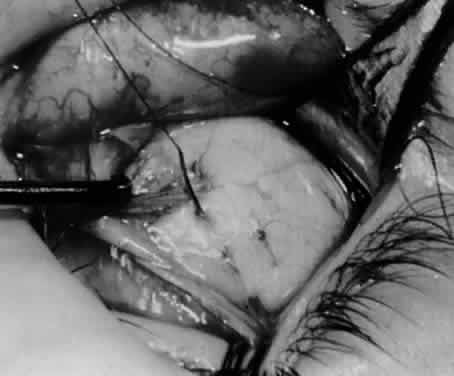
The denervation procedure (Figs. 21–32) allows the inferior oblique muscle to be released further into the operative field once the nerve has been sectioned (see Figs. 26 and 27). A 3-0 Vicryl suture ligature is placed around the inferior oblique muscle (see Fig. 28) as close to the Tenon's capsule penetration as possible. The inferior oblique is sectioned by cautery (see Fig. 29), just distal to the suture ligature. The cauterized stump is pushed through the opening in the Tenon's capsule (see Figs. 30 and 31) and a 6-0 or 7-0 Vicryl suture is used to close the opening, with either a running or a purse-string suture (see Fig. 32). The purse-string suture can be preplaced before the inferior oblique muscle is sectioned and closed after the muscle is sectioned. The advantage of the denervation and extirpation procedure is its ability to permanently correct 4+ overaction of the inferior oblique.10,18 In addition, it is the best operative procedure to eliminate recurring inferior oblique overaction after disinsertion, myectomy, or recession.10 Disadvantages include permanent underaction of the inferior oblique muscle in some patients. Pupil dilation can occur but the dilation usually is transient, clearing in 3 to 6 months.10,18
|
|
|
|
|
|
|
|
ANTERIOR TRANSPOSITION
Elliott and Nankin19 modified the standard recession procedure by transposing the inferior oblique muscle anteriorly toward the insertion of the inferior rectus muscle (Figs. 33–35). This procedure reduced the persistent inferior oblique overaction that frequently is noted after recession surgery and reduced marked inferior oblique overaction when performed as the initial surgical procedure. Seventy-three percent of patients, however, had a postoperative deficiency in primary position elevation, compared with only 25% who underwent the usual inferior oblique recession surgery. Bremer and coworkers20 performed a recession and anteriorization of the inferior oblique muscle on 3 patients who had fourth nerve palsy. They suggested that this procedure would benefit patients with dissociated vertical deviations because the inferior oblique is converted to a depressor muscle by the anterior transposition. Ziffer and associates21 also suggested that the anterior transposition converts the inferior oblique muscle from an elevator to a depressor on attempted elevation. Because of its powerful weakening ability, the anterior transposition should be reserved for patients with moderate to severe inferior oblique muscle overaction and should be performed on both eyes to avoid postoperative hypotropia in upgaze. Gonzalez and Cinciripini22 proposed the anterior transposition procedure for treatment of unilateral superior oblique palsy. None of their 3 patients developed primary position hypotropia but all demonstrated some elevation deficiency, with elevation of the lower lid in upgaze.
|
Stager and coworkers23 described clinical, radiologic, and histologic evidence that the neurovascular bundle supplying the inferior oblique muscle serves as the functional origin of the inferior oblique after anterior transposition of the insertion and converts the distal portion of the inferior oblique muscle from an elevator to a depressor. Stager and Weakley24 described a new surgical approach for management of recurrent inferior oblique overaction after the anterior transposition procedure. A myectomy of about 1 cm or more of a portion of the inferior oblique, nasal to the inferior rectus, is performed using a temporal incision and approach. This preserves the distal inferior oblique fibers attached to the neurovascular bundle, which provide the depressor function of the inferior oblique in its anterior transposed position.
Mims25 performed an anterior transposition on 61 children who had bilateral overaction of the inferior oblique muscle with concurrent or previous infantile esotropia. A substantial reduction in the dissociated vertical deviation occurred in all cases when it was present, and only one child required subsequent surgery for dissociated vertical deviation. In a prospective study, Elliott and Parks26 compared the effectiveness of denervation and extirpation with that of anterior transposition in the management of patients who had maximum inferior oblique overaction. They concluded that the anterior transposition procedure was effective for eliminating bilateral superior oblique overaction but that it should be performed identically on both eyes because of its tendency to restrict elevation. The anterior transposition procedure was recommended for the treatment of patients with overactive inferior oblique muscles in association with dissociated vertical deviation. In a series of 21 patients receiving an anterior transposition of the inferior oblique with overaction of the inferior oblique and dissociated vertical deviation, Seawright and Gole27 reduced the preoperative incidence of inferior oblique overaction from 84% to 16% postoperatively. Inferior oblique overaction was absent in 43% and improved in 86% of eyes. At the latest postoperative visit, 57% did not demonstrate any evidence of dissociated vertical deviation and 68% of eyes had no dissociated vertical deviation or improved dissociated vertical deviation. There was no evidence of primary position hypotropia in any patient who had unilateral anterior transposition, and there was no evidence of inferior oblique underaction. Three patients required repeat inferior oblique surgery.
Burke and colleagues28 also found the anterior transposition of the inferior oblique to be an effective treatment for dissociated vertical deviation with inferior oblique overaction but the long-term results may be less stable if the preoperative dissociated vertical deviation is in excess of 15 prism diopters.