The Goldmann tonometer is used in conjunction with a slit-lamp biomicroscope to which one of two types of Goldmann tonometers can be attached. The following description is written with the Haag-Streit slit lamp in mind. The principles may easily be applied to other biomicroscopes.
The slit lamp is adjusted for the examiner. Low-power oculars are preferable, and the objective lens is also set at its lowest power. The examiner may choose to align the optical portion of the tonometer with either the left objective or the right objective of the biomicroscope, depending on his own ocular dominance. The front surface of the prism is wiped with water and dried with a clean tissue. Hexachlorophene or other detergents should not be used, since residue on the prism may be toxic to the cornea. The biprism is adjusted such that the interface between the two prisms is oriented horizontally. If a high degree of corneal astigmatism is present in the subject's eye, the axis of the interface should be set 43° from the flattest axis of the cornea.
The examiner estimates the pressure in the eye and sets the dial of the tonometer to the estimated pressure. (The scale reading in grams multiplied by 10 equals the pressure in millimeters of mercury.)
The blue filter is introduced into the light path, and the slit is opened to its widest position. The light must be sufficiently oblique from either side to illuminate the tip of the prism and not cause interfering reflections.
Corneal anesthesia is required for accurate tonometry in most subjects. Proparacaine hydrochloride 0.5% is suitable. After instillation of the anesthetic, fluorescein can be added to the tear film by touching the everted lower tarsal conjunctiva with a moistened strip of fluorescein-impregnated paper. Alternatively one can use an anesthetic such as 0.4% benoxinate hydrochloride, which contains 0.25% fluorescein sodium. In either case it is not necessary to use more than a small amount of fluorescein to observe the inner margins of the meniscus of contact between the cornea and the tonometer. If argon laser treatment is to follow tonometry the same day, the least amount of fluorescein should be applied that permits visualization, and the fluorescein should be washed away with an irrigating solution immediately after tonometry. (Fluorescein absorbs the 488-nm wavelength of argon lasers.) If anesthetics cannot be instilled because of allergy, an experienced examiner can warm the tip with water to slightly above body temperature and perform tonometry without anesthesia.
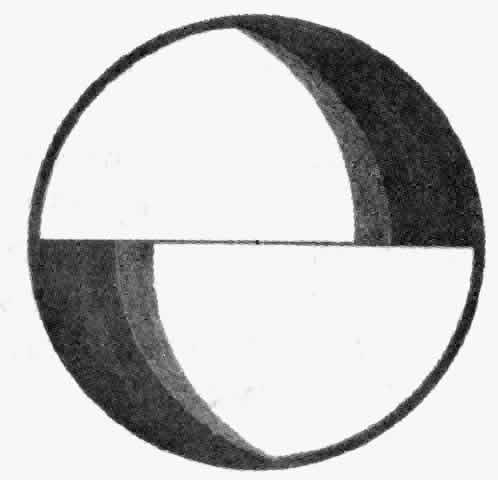
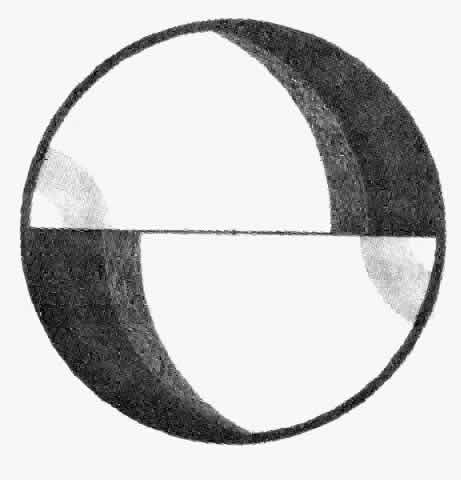
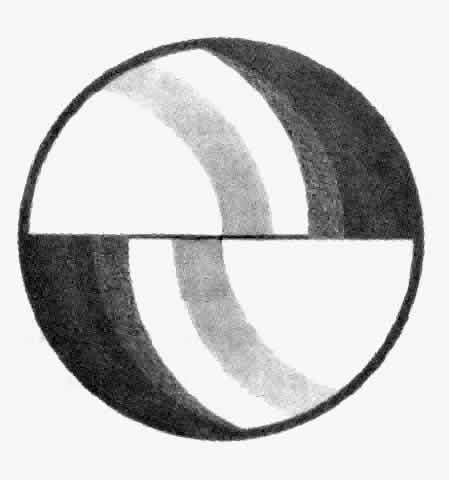
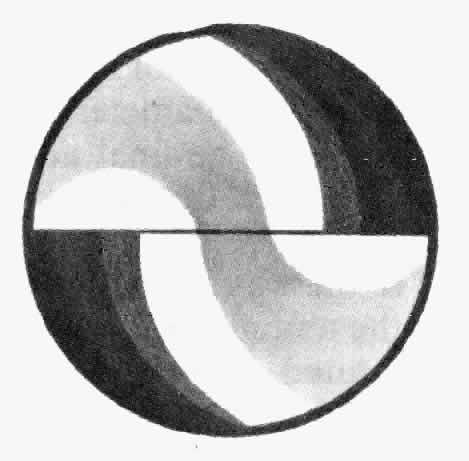
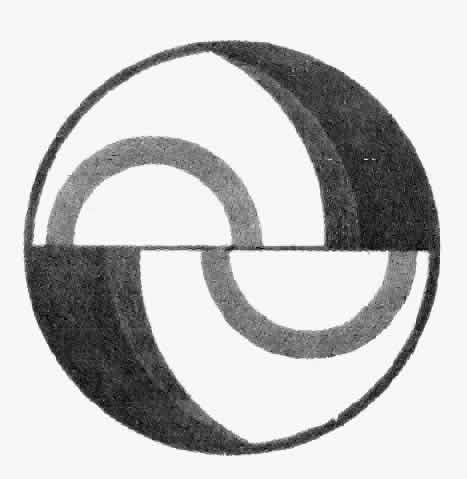
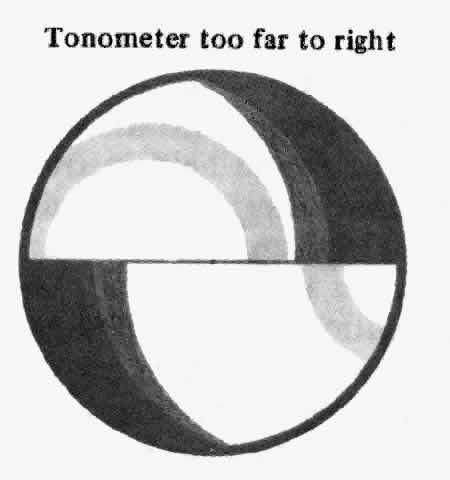
The slit lamp is adjusted so that the patient is comfortable. A tight collar or necktie should be loosened. The patient is asked to stare straight ahead and to resist the natural tendency to blink. The slit lamp is moved in order to approach the cornea along the optic axis. With the joystick held back, the entire examining unit of the slit lamp (including the tonometer) is moved to a position approximately 2 mm to 3 mm anterior to the cornea. The initial position should be inferior to the visual axis in order to make it possible to slip under the eyelashes of the upper lid without touching them. If necessary the upper lid should be lifted gently. The tonometer is then raised until the prism is centered. At this point the examiner begins to look through the biomicroscope. The reflected image of the tip of the tonometer can be used to guide the alignment of the tip even before contact is made. The image appears as hint purple arcs that move as the position is adjusted. When these arcs appear symmetric in the two halves of the biprism, the instrument is aligned correctly (Figs. 1 THROUGH 9). The joystick is moved forward slowly. Just before the corneal surface is touched, the arcs will meet.
|
|
|
|
|
|
|
|
|
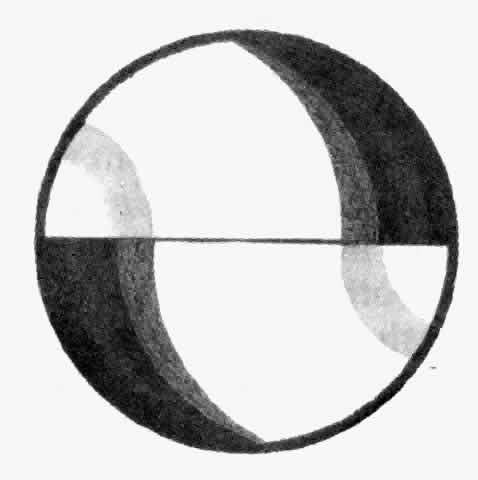
When the corneal surface is touched, two bright green semicircles appear. These semicircles should be in the proper position when they first appear. If not, the joystick should be pulled back, the tonometer wiped, and the process repeated. The subject must blink between applications to keep the cornea moist. This step is especially recommended for inexperienced examiners. If the cornea is only slightly out of line, the alignment can be adjusted without withdrawing the tonometer.
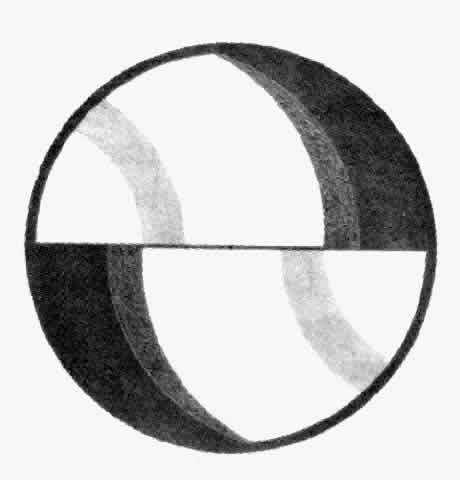
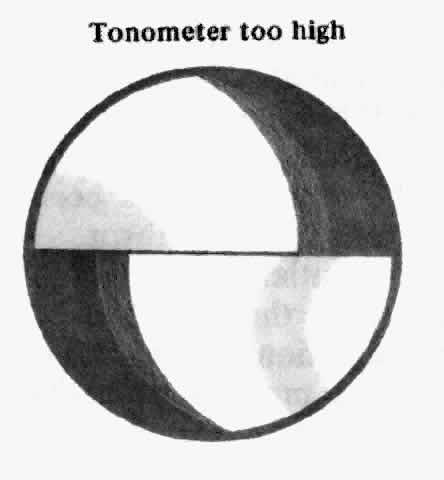
The two halves of the meniscus of contact, the inner margins of which delineate the flattened area, are observed. These semicircles should be symmetric, bright, and sharply focused. The tonometer dial is adjusted so that the inner edge of the superior semicircle meets the inner edge of the inferior semicircle exactly. Pulsatile changes in the diameter of the semicircles are usually observed. The final adjustment can be made halfway between the two extremes of the pulse.
If an eyelash has “strayed” in the way so that one of the semicircles is distorted, the tonometer is withdrawn and the examination repeated. If there is too much or too little dye present, the problem should be corrected. If a diffuse greenness is noted in the entire area where the prism is in contact with the cornea, the cornea may have been abraded and tonometry may not be accurate. If the semicircles overlap markedly and their size does not change as the tonometer dial is turned, the tonometer has been pushed too far forward and must be withdrawn.
It is recommended that after initial determination of the pressure of each eye is made the procedure be repeated. If the second determination of intraocular pressure differs by more than 1 mm Hg from the first, a third measurement is made. Consecutive measurements of a given eye should differ by no more than 1 mm Hg.
The prism is wiped with water and dried with a clean tissue. The tonometer is stowed so that no pressure is placed on the torsion balance. On certain slit lamps the tonometer can be swung to the side or the tonometer arm swiveled into its holder.
Use of the Perkins tonometer differs in certain particulars from use of the Goldmann instrument. The newcomer to Perkins tonometry will find that the intraocular pressure will seem to be slightly lower with the hand-held instrument than with the slit-lamp instrument. After a little practice, the two instruments can be made to agree fairly closely. It is advisable to use a slightly greater concentration of fluorescein when employing the hand-held instrument in order to make the inner margin of the tear wedge easier to observe. It is also mandatory that the room be darkened and that fresh batteries be used so that adequate illumination is available during tonometry. The examiner must be careful not to allow the meniscus of the biprism to mingle with either the superior or inferior tear meniscus of the lid margins. An excess of tears or mucus will obscure the end point and lead to large errors. This precaution is especially important when examining the eye in the first few days after surgery. It is also important that the lids and lashes not touch the tonometer. If the cornea is astigmatic, it is advisable to measure the pressure at two orthogonal orientations of the biprism and average them. In patients with abnormal extraocular muscles and deviations, such as dysthyroid ophthalmography, the Perkins tonometer can be used to measure the pressure in the position of greatest muscle relaxation and avoid artifacts due to ductions against retracted muscles.
The Mackay-Marg tonometer must be used skillfully with a technique that is not easy to master. It is important that the instrument be calibrated regularly against an absolute standard. This procedure is necessary to eliminate errors due to accumulation of residues between the sensitive plunger and the insensitive footplate. For daily use the instrument can be calibrated against the weight of its own plunger. These procedures assure the examiner that mechanical and electrical drift do not affect the accuracy of the reading. It is also helpful from time to time to compare Mackay-Marg readings with Goldmann readings in subjects with normal corneas. If the instrument is used regularly the technique can be mastered. If the baseline is set properly the instrument can be used in any position from vertical to horizontal.
The most common mistake when using the Mackay-Marg tonometer is to move the tip back and forth too rapidly. Rapid movements impart significant forces on the pressure-sensing transducer as a result of inertia. The rate of back and forth motion of the tonometer should be slow enough that if performed in air without touching the eye no visible oscillations will be present on the tonometric tracing. The instrument is then applied to the cornea as smoothly and evenly as possible and at right angles to the corneal surface. A slight indentation of the cornea is required to be certain that the instrument is properly coupled to the eye. Unsteadiness either of the patient or of the head of the examiner or too slow an application and withdrawal can produce artifacts in the tracing. These artifacts must be discriminated from true end points. A number of consistent end points must be observed before concluding that the reading is accurate.
Mackay-Marg readings will tend to be high in comparison with Goldmann readings. This situation is exaggerated when the cornea is abnormal or if the tonometer is used incorrectly. When the cornea is excessively scarred or thick, no tonometer can measure intraocular pressure with sufficient accuracy to satisfy clinical needs.
The Bigliano tonometer8 has been available to clinicians in two forms. The earlier form, marketed under the trade name Applamatic, was difficult to use and offered no advantages over the Mackay-Marg tonometer. An important modification was made by Webb,9 who devised a gas bearing and floating tip, which facilitated the application of the tonometer to the eye and permitted the tonometer to make a continuous recording of intraocular pressure. The instrument is available commercially under the trade names Pneumatonometer* and Pneumatonograph.†
* Digitals, Cambridge, MA.
† Alcon Laboratories, Fort Worth, TX.
These instruments are easy to use for performing tonometry in humans. If calibrated according to the manufacturer's recommended method, tonometry can be performed in human subjects in the sitting position. The tonometer tip is brought against the anesthetized cornea until a high-pitched sound is heard and the pressure is read from an LED display or from a graph. In normal human eyes this tonometer tends to read high at low intraocular pressures and low at high intraocular pressures, and thus its range is compressed toward normal pressures.12
The reader is cautioned that a number of papers have been published in which it is concluded that this instrument is an applanation tonometer that follows the Fick-Imbert law, that it can be used in any position without a correction for gravity, and that it is a low-displacement tonometer. These conclusions have not been confirmed by the most meticulous studies of the instrument.12 Nevertheless this tonometer provides an objective reading, permits a continuous recording of intraocular pressure, and is simple to use. For these reasons it is among the best tonometers for clinical research in which an unbiased measurement of changes of intraocular pressure is needed in human or in animal eyes. When used for measurement of intraocular pressure in animal eyes, the instrument must be recalibrated. At the least, the instrument must be calibrated against the eye of the species to be tested using the closed-stopcock method. In some animals with very flexible corneas such as the rabbit, it is preferable to reduce the rate of gas flow by removing the cover of the instrument and adjusting the regulator until the gas bearing is barely functional. The recalibrated instrument is then more reliable for use in these species.