ROUTINE
Vision
The vision is an integral part of any orbital examination. Visual acuity provides an indicator of the extent of orbital disease, and decreased vision suggests involvement of the optic nerve or globe. Vision gives a baseline from which to measure progression of disease and is a medical-legal necessity. This is even more important in patients presenting with orbital trauma. It is vital to perform a visual acuity examination before taking trauma patients to surgery even if this requires using a Desmarres retractor to open the swollen eyelids. Nonophthalmic surgeons who are called on to operate for trauma in the orbital area frequently neglect this vital part of the orbital examination.
Pupils
Examination of the pupils is very important and may provide information about the underlying orbital condition. The small pupil of a Horner's syndrome may be the clue that one is dealing with a pseudoenophthalmos. The large pupil of a third cranial nerve palsy indicates that the associated diplopia is due to a paralytic abnormality as opposed to a restrictive phenomenon. The presence of a relative afferent pupillary defect is confirmation that the optic nerve is compromised by orbital disease, even though many patients have an optic nerve head that appears normal on funduscopic examination.
Extraocular Movements
The cross cover test is invaluable for assessing ocular position in primary position, upgaze, downgaze, right gaze, and left gaze. In most orbital disorders the deviation will vary in different positions of gaze. The nonconcomitance of strabismus associated with orbital disease helps to distinguish it from other common forms of strabismus. It is important to note abnormal ductions because a slight limitation in one eye may be the only evidence of an abnormality and may be very useful in localizing the orbital lesion.
Slit-Lamp Examination
Slit-lamp examination is most useful for assessing the status of the cornea that may demonstrate exposure keratopathy caused by proptosis or lid retraction. Many orbital disorders cause dilatation of conjunctival vessels and conjunctival edema. These findings are relatively nonspecific, but large tortuous conjunctival veins may be a sign of carotid cavernous fistula.
Intraocular Pressure
Intraocular pressure may be elevated in patients with orbital disease, through a variety of mechanisms. Carotid cavernous fistulas cause an increase in episcleral venous pressure and, therefore, impede aqueous outflow. Mass lesions may press directly against the globe, especially when a retrobulbar hemorrhage causes a sudden expansion of the mass. Restriction of the extraocular muscles, such as may occur with blowout fracture or thyroid eye disease, produces a factitious elevation of intraocular pressure when the eye attempts to rotate against the restricted muscle. In cases of mild thyroid eye disease, the progressive increase in intraocular pressure with elevation of the eye may help to confirm the diagnosis.
Fundus Examination
Fundus examination is important to assess the optic nerve. Tumors may compress the optic nerve, causing disc edema or optic atrophy. Optic nerve meningiomas may produce shunt vessels on the disc. Choroidal striae may be noted if a mass is indenting the globe. On occasion intraocular tumors may extend through the sclera into the orbit, and the correct diagnosis is made when the intraocular tumor is identified.
Color Vision
Assessment of color vision is an important test for optic nerve dysfunction, although one must be careful not to attribute optic nerve dysfunction to patients who have a congenital abnormality of color vision. Sophisticated tests for color vision measurement, such as the Farnsworth-Munsell test, are not generally required for clinical assessment of optic nerve dysfunction. The Ishihara color plates are satisfactory for clinical use.
SPECIALIZED ORBITAL EXAMINATION
Inspection
Inspection of the face and more specifically the periocular adnexa is the simplest of all examinations and yet this inspection is frequently overlooked by neophyte examiners. It is important to look at the entire face to get a sense of the facial proportion and symmetry.
Globe Displacement
Globe displacement (horizontal or vertical) does not always result in diplopia. Even so, patients may present with the complaint that the eye does not “look right.” It is important to determine whether the apparent displacement of the globe is real or illusory. Posttraumatic telecanthus or large congenital epicanthal folds may create the false impression that eyes are displaced medially. Tripod malar fractures may produce a displacement of the lateral canthal complex and the illusion that the eye is abnormally positioned, when the true anatomic abnormality involves the zygoma and eyelids. Vertical displacement of the globe is frequently seen after blowout fractures or orbital decompression. Orbital roof fractures or tumor masses present in the superior orbit may cause the globe to be displaced inferiorly. This displacement may or may not be associated with ipsilateral ptosis and/or decreased supraduction. The horizontal position of the globes is measured from the center of the bridge of the nose using a ruler to determine the distance from the midline to the center of the pupil (Fig. 1). Previous trauma or surgery to the nose may make this measurement unreliable. Vertical displacement of the globe is evaluated by placing a ruler in a horizontal position across the bridge of the nose. The relative positions of the globes may be assessed and the vertical displacement can be either measured or estimated in millimeters. Once again significant trauma to the midface renders this measurement inaccurate.
|
Color
The color of the eyelids may provide a clue to the underlying orbital pathology. In many cases there will be no discoloration of the eyelids. However, inflammatory lesions often cause an erythema of the eyelids. This redness may be associated with edema and tenderness. Bruising of the eyelids is most frequently seen following trauma but may be associated with hemorrhage into an underlying orbital lesion. Spontaneous hemorrhage most frequently occurs with lymphangioma and hemangioma but may be seen with other tumors, such as childhood neuroblastoma. Lymphangiomas and deep seated hemangiomas have a bluish tint. More superficial vascular lesions are red or maroon.
Pulsations
Pulsation of the eyelids and orbital contents is an infrequent finding and may be easier to appreciate with palpation rather than visual inspection. Pulsation is most commonly seen in neurofibromatosis, in which the absence of sphenoid bone allows brain pulsations to be transmitted to the orbital contents. Extremely vascular tumors may occasionally pulsate because of the high blood flow in these lesions.
Palpation
Palpation of the orbit is a simple maneuver that often provides important information. The upper and lower eyelids should be palpated gently. It is possible to insert the tip of a small finger between the globe and the orbital rims on all four sides so that the anterior orbital contents may be palpated. In this way abnormalities of the lacrimal gland or the lacrimal sac can be identified, and abnormalities of the orbital rim are easily appreciated. This technique is especially useful for trauma patients who may have a step deformity of the orbital rim.
Retropulsion of the globes is a test that has received considerable attention. This test is performed by placing the fingers over both eyes and gently pushing them in a posterior direction. A firm lesion present behind the globe will resist retropulsion and this sensation is palpable. Unfortunately, this test is nonspecific and has little diagnostic value.
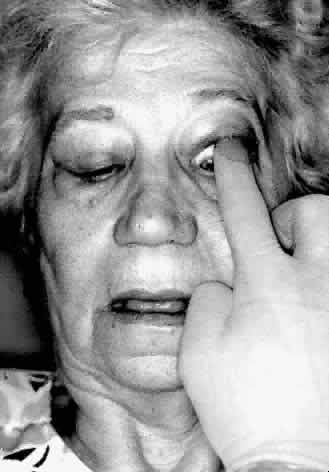
Digital examination of the superior fornix is a particularly useful technique for evaluating superior orbital lesions. To perform this examination the conjunctival sac is anesthetized with a topical agent. A gloved finger is gently inserted behind the upper eyelid into the superior fornix (Fig. 2). The finger is moved medially and laterally and anteriorly and posteriorly to palpate any lesions present in the superior part of the orbit. Bimanual palpation is sometimes helpful (Fig. 3). It is useful to have the patient look down during the examination because this position is more comfortable. In addition, downward rotation of the globe will sometimes bring an orbital mass more anteriorly so that it may be more readily palpated. Small orbital rim fractures may also be identified in this way. Lacrimal gland abnormalities may be easily palpated. This technique is particularly useful if the upper eyelid is swollen, making palpation of the orbital mass through the eyelid difficult. The same technique may be used in the inferior fornix.
|
Sensation
The first and second divisions of the trigeminal nerve provide sensation to the face in the orbital area. The ophthalmic branch provides sensation in the forehead, upper lid, and globe, whereas the maxillary division via the infraorbital nerve gives sensation to the cheek and upper lip. Sensation is usually tested by touching these areas with a wisp of cotton and asking if the patient is able to feel the touch. It is useful to compare one side to the other because the sensory deficit is incomplete in many cases of orbital disease. Hypoesthesia of the cheek and lip is a typical finding in patients with blowout fractures because of injury to the infraorbital nerve as it travels through its bony canal in the orbital floor.
Exophthalmometry
Exophthalmometry is an accurate technique for the measurement of proptosis. This measurement may be accomplished in several ways, but in each case the reference points are the lateral orbital rim and the apex of the cornea. The generally accepted normal value is less than 22 mm. However, there are some patients without orbital disease who have exophthalmometry readings greater than 22 mm. The absolute value of the exophthalmometry reading is less important than the difference between the two eyes. The left and right measurements should not differ by more than 2 mm.
Exophthalmometry may be performed with a Hertel type of instrument. This instrument rests against the lateral orbital rim and the position of the corneal apex is measured by means of mirrors (Fig. 4). Frueh has shown that inexperienced examiners give less reliable measurements than experienced examiners.19
|
Although the Hertel exophthalmometer is the most widely used instrument, exophthalmometry readings may be obtained by simply placing a transparent ruler on the lateral orbital rim and measuring the position of the cornea. Inspection from behind the patient looking over the forehead down onto the proptosed globes is also a way to estimate proptosis (Fig. 5).
|
Forced Duction Test
The forced duction test is a useful test for distinguishing paralytic strabismus from restrictive strabismus. The forced duction test is used to detect an inelastic extraocular muscle that prevents the globe from rotating. For example, a tight inferior rectus muscle will not allow the globe to rotate superiorly. The test is carried out by placing topical anesthetic into the conjunctival sac. The globe is grasped with a pair of toothed forceps at either the limbal area (where Tenon's capsule is tightly adherent to the globe) or the insertion of the extraocular muscle, and an attempt is made to “force” the globe to rotate in the desired direction (Fig. 6). Restriction may be felt when the globe reaches the end of its “tether.” (For some patients, especially in the pediatric age group, application of the forceps to the globe is too frightening or painful. In these situations the forceps may be replaced with a cotton swab and the globe gently pushed.) The forced duction test is particularly useful for differentiating between a medial wall blowout fracture with medial rectus entrapment and a sixth cranial nerve palsy.
Auscultation
Auscultation of the orbit will detect bruits. Orbital bruits are generally due to high flow, high-pressure carotid cavernous fistulas, or in some cases high-flow arteriovenous malformations. The examiner must be careful to ensure that the fellow eye remains in primary position during auscultation because ocular movements behind the closed eyelid cause noise that can be readily heard through the stethoscope.
Nasal Examination
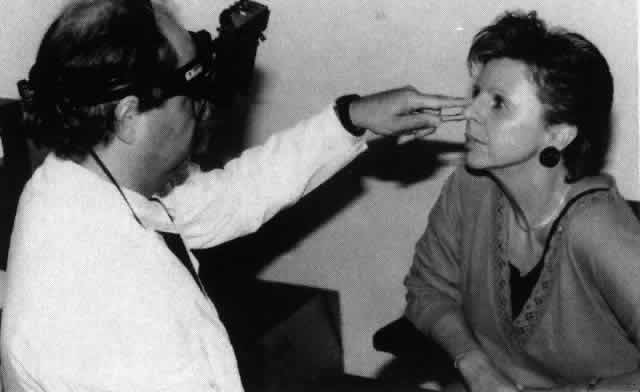
Nasal examination is a useful technique for the orbital surgeon because nasal or sinus inflammation and tumors sometimes have an orbital presentation. The nasal mucosa is anesthetized and decongested with 5% cocaine spray (or something similar). When the nasal speculum is inserted into the nose it is helpful to hold the external naris with the index finger to stabilize the speculum. Nasal visualization is carried out by means of the time-honored center-hole head mirror. However, the indirect ophthalmoscope is an excellent tool for looking into the nose and gives the examiner the added advantage of binocularity (Fig. 7).
Nasal endoscopy is another excellent way of examining the nose. The nose is similarly prepared and the endoscope is placed into the nostril. Visualization is much easier using a camera and monitor than looking directly though the endoscope. In addition, photographic documentation of nasal abnormalities is possible (Fig. 8).
|