|
The optical accessibilities and properties of the eye are compatible with PDT. Visible light is transmitted to the retina with little absorption loss.14 All anterior segment components essentially are nonscattering, thus allowing their functioning as high-quality optical elements. In contrast, the sclera is highly scattering for the light reflecting from the retina and choroid. The effect of its back-scattering into the eye is diminished greatly by the pigmented epithelial layer.
PDT typically is performed with lower irradiances than those used in thermal laser photocoagulation, such as 150 to 200 mW/cm2, levels at which photochemistry predominates over thermal mechanisms. Mild hyperthermia may be produced at greater irradiances (e.g., 600 mW/cm2). If the optical power densities and energy densities are high enough, then a significant temperature increase can be produced in the exposed tissue, as in laser retinal photocoagulation. Synergism between PDT and hyperthermia has been reported by numerous investigations.15,16
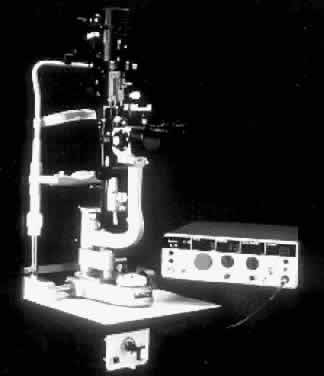
Practical considerations and differences in performing PDT treatment via the slit lamp versus thermal laser photocoagulation are the use of lower irradiance and power levels, longer durations of light application, and increased spot sizes. Because the duration of light ranges from seconds to minutes, proper alignment of the activating light beam must be maintained. Because the intensity of the light therapy is low, patients appear to tolerate the prolonged light treatment. In patients unable to fixate because of poor vision in the fellow eye, retrobulbar anesthesia for akinesia occasionally may be necessary. Typical powers required for PDT range from 5 to 50 mW, covering beam diameters of 0.5 to 3 mm spot sizes. Table 2 provides definitions and abbreviations for light terminology used in the treatment.
TABLE 69C-2. Light Terminology: Definitions and Abbreviations
Joule (J): Unit of energy equivalent to 1 watt-second.
Light dose: The total amount of energy given per unit area of surface treated. It
is determined by multiplying power density (W/cm2) and treatment duraction (sec). It is expressed in J/cm2.
Milliwatt (mW): Power equivalent to 1 watt/1000. A watt is a unit of power equivalent
to the amount of energy (J) given off each second (sec).
Power density: The power density, also known as irradiance, is defined as the power (mW) delivered
to the tissue divided by the area (cm2) of the tissue being irradiated. It is determined by dividing the light
dose (J/cm2) by the treatment duration (sec). It is expressed in mW/cm2.
Power output: Power of light emitted through an optical fiber. It is a measurement of
the rate at which energy is delivered. The number of watts (W) equals
the amount of energy (J) given off each second (sec).
Treatment time: The duration of time required for the light treatment; expressed in seconds (sec). It
is equivalent to the light dose (J/cm2) divided by the power density (mW/cm2).
Treatment area: Total surface area exposed to light during photodynamic therapy treatment. It
is equivalent to π(radius)2 and is expressed as square centimeters (cm2).
Radius (r): Radius of the light field. It is expressed in centimeters (cm).
Diameter (d): Diameter of the light field. It is expressed in centimeters (cm).
Area (A): Area of the light field. It is equivalent to π(radius)2 and is expressed as square centimeter (cm2).
Wavelength: The wavelength is the distance between corresponding points on successive waves. It is expressed in nanometers (nm).