The use of goniolenses of this type (Koeppe) constitutes the direct method
of gonioscopy. Since these goniolenses have a steeper curvature than
the cornea, there is a space between the inner surface of the lens
and the cornea, This space is filled with methylcellulose, saline, or
some other solution. For all practical purposes this solution creates
an optical continuity between the lens and the cornea (Fig. 3). The more steeply curved outer surface of the gonioscopy lens replaces
the cornea-air interface, thus altering the critical angle and permitting
visualization of the angle. The chamber angle is observed by viewing
directly across the anterior chamber. A true image is seen with true
spacial orientation. Magnifying loops, a hand-held microscope, or
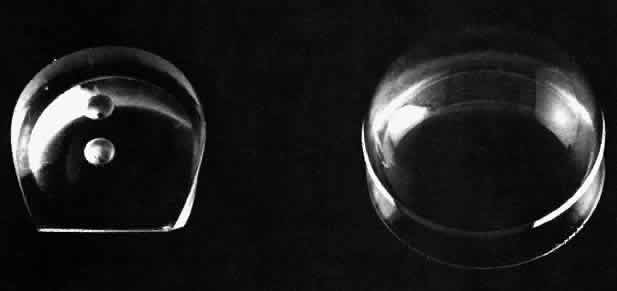
an operating microscope is used to magnify the image viewed (Fig. 4); the gonioscopy lens itself provides about 1.5 x magnification. Fig 3. Schematic drawing of a direct gonioscopy lens. The steeper radius of curvature
of the gonioscopy lens is substituted for that of the cornea, permitting
direct visualization of the angle recess. Note the fluid bridge
between the cornea and the gonioscopy lens, which links them functionally
into a single optical system. Fig 3. Schematic drawing of a direct gonioscopy lens. The steeper radius of curvature
of the gonioscopy lens is substituted for that of the cornea, permitting
direct visualization of the angle recess. Note the fluid bridge
between the cornea and the gonioscopy lens, which links them functionally
into a single optical system.
|
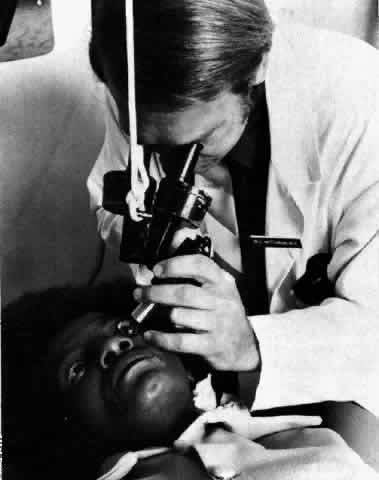
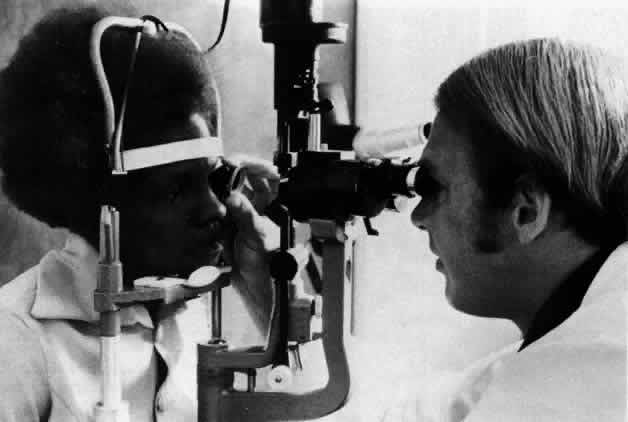
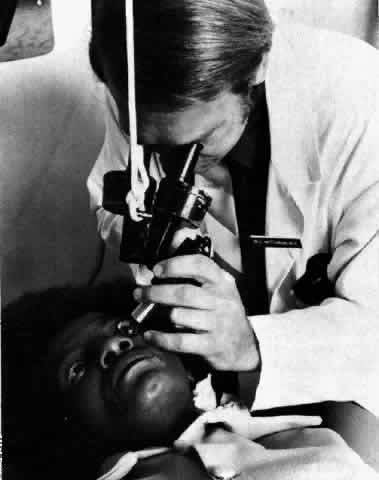 Fig 4. Performance of direct gonioscopy. The hand-held microscope is partially
supported by a counterweight, and illumination is supplied by a separate
illuminator. Fig 4. Performance of direct gonioscopy. The hand-held microscope is partially
supported by a counterweight, and illumination is supplied by a separate
illuminator.
|
MIRRORED Mirrored gonioscopy lenses were introduced by Goldmann in 1938. The optical
power of the front surface of the cornea is essentially eliminated
by the lens, and an angulated mirror is placed within the lens. The
mirror reflects the light rays originating from the chamber angle recess
to the line of vision of the viewer (Fig. 5). Because of this reflection system, the image seen is inverted and is
projected 180° away from where it originates. Since the image is
inverted, this type of gonioscopy is referred to as indirect gonioscopy. (There is at least one mirrored gonioscopy lens that has a
double-mirror system, resulting in an erect rather than an inverted image.) The
mirrored gonioscopy lenses are generally used in conjunction
with a slit lamp; the slit-lamp microscope provides the magnification, and
the slit beam provides the illumination (Fig. 6).  Fig 5. Schematic drawing of an indirect gonioscopy lens. The light ray originating
from the angle recess is reflected by the mirror inside the lens. Fig 5. Schematic drawing of an indirect gonioscopy lens. The light ray originating
from the angle recess is reflected by the mirror inside the lens.
|
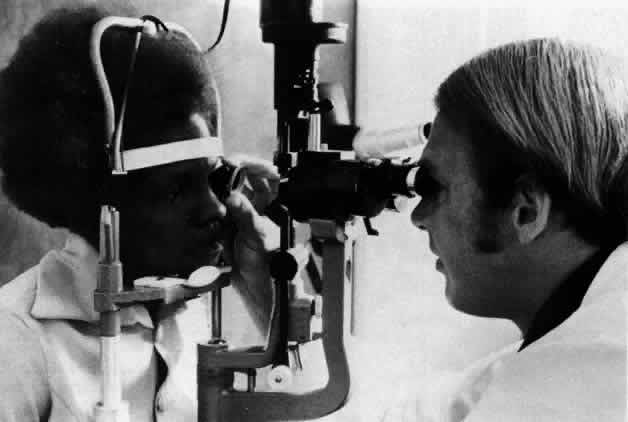 Fig 6. Performance of indirect gonioscopy. The slit lamp provides both magnification
and illumination. Fig 6. Performance of indirect gonioscopy. The slit lamp provides both magnification
and illumination.
|
At the present time there are a number of mirrored gonioscopy lenses that
are available commercially. Some of the differences that distinguish
these lenses from one another are the number of mirrors, the angulation
of the mirrors, the location of the mirror relative to the apex of
the cornea, the diameter of the base of the lens, and the radius of curvature
of the lens. Some of the practical implications of these differences
will be discussed below. Most gonioscopy lenses have their mirrors set at an angle of 59° to 64° from
the horizontal plane, with 62° being the most common. Those
lenses that also have mirrors intended to be used for examining
the ora serrata and peripheral retina have mirrors with steeper angles. They
may be as steep as 80°. In the one- or two-mirror Goldmann-type
lenses, the mirror is positioned approximately 3 mm from the apex
of the cornea when the lens is perfectly centered. In contrast, in
a three-mirror Goldmann-type lens, the mirror is 7 mm from the center
of the cornea. This means that the viewing angle across the anterior chamber
is considerably flatter. In an eye with iris bombé, it may
not be possible to see over the convexity of the iris into the angle
with a more peripherally placed mirror, while the angle may be visible
with a more centrally placed mirror (Fig. 7).  Fig 7. Schematic drawing showing how the relation of the mirror to the apex of
the cornea may determine whether the angle recess can be visualized in
eyes with a marked convexity of the iris. Fig 7. Schematic drawing showing how the relation of the mirror to the apex of
the cornea may determine whether the angle recess can be visualized in
eyes with a marked convexity of the iris.
|
The Goldmann lenses have a radius of curvature of 7.4 mm, which is steeper
than the normal cornea. The Zeiss four-mirror lens (and other similar
lenses) has a somewhat flatter base with a 7.85-mm radius of curvature. Because
of this the Zeiss lens is used with just the normal tear
film as a liquid bridge between the lens and cornea, while the Goldmann-type
lenses require the use of a more viscous bridge such as methylcellulose. The
Zeiss lens has a much smaller diameter base (Fig. 8). Its internal diameter is 9 mm, or in other words less than the corneal
diameter. The one- or two-mirror Goldmann lenses have a 12-mm internal
diameter. The three-mirror Goldmann lenses have a diameter of 15 mm.  Fig 8. Front and back views of the Zeiss four-minor gonioscopy lens. Fig 8. Front and back views of the Zeiss four-minor gonioscopy lens.
|
With the one-mirror Goldmann-type lens, and to a much greater extent with
the Zeiss lens, it is possible to place pressure on the limbus or to
indent the cornea and distort the anatomy of the anterior chamber (Fig. 9). In this manner it is possible to open artificially an angle that has
appositional closure. Used properly, this ability to manipulate the peripheral
iris and angle purposefully can be quite helpful in differentiating
between appositional and synechial closure of the angle. (This
technique of identation gonioscopy using the Zeiss four-mirror goniolens
has been well described by Forbes.2)  Fig 9. Use of indentation gonioscopy to differentiate between appositional and
synechial angle closure. (A) Eye with angle closure. (B) With indentation
gonioscopy, aqueous is forced peripherally, opening the appositional
closure. (C) The synechial closure is not affected by the indentation
even though the peripheral iris is pushed posteriorly. Fig 9. Use of indentation gonioscopy to differentiate between appositional and
synechial angle closure. (A) Eye with angle closure. (B) With indentation
gonioscopy, aqueous is forced peripherally, opening the appositional
closure. (C) The synechial closure is not affected by the indentation
even though the peripheral iris is pushed posteriorly.
|
On the other hand, if one artificially distorts the angle and is unaware
of it, a false impression of the anatomy can be obtained. THERAPEUTIC The initial therapeutic use of gonioscopy lenses was in conjunction with
the performance of goniotomy operations. Although the basic technique
had been described much earlier, Barkan popularized the use of this
technique and obtained the excellent results that he did because he was
able to see the angle structures accurately and incise them very superficially
with his knife. This technique demanded a lens that left space
over pan of the cornea for entry with the goniotomy knife yet provided
a view of a significant portion of the angle so that at least 3 dock
hours could be treated. Barkan solved this problem by designing a
sort of truncated, partial Koeppe lens that included two small dimples
on its surface, which could be used for stabilizing or manipulating the
lens (Fig. 10). Worst designed a somewhat different lens that was actually sutured to
the globe for stabilization but included a small aperture in the lens
to allow for introduction of the goniotomy knife (Fig. 11). 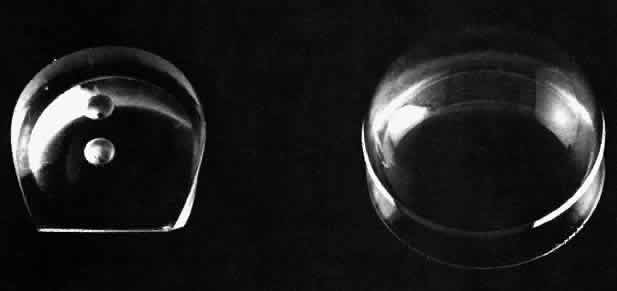 Fig 10. A Barkan goniotomy lens (left) next to a Koeppe-type direct gonioscopy lens. Fig 10. A Barkan goniotomy lens (left) next to a Koeppe-type direct gonioscopy lens.
|
 Fig 11. Goniotomy being performed with a Worst goniotomy lens. The lens is sutured
to the globe for stability, and the needle-knife is passed through
the opening in the lens. Fig 11. Goniotomy being performed with a Worst goniotomy lens. The lens is sutured
to the globe for stability, and the needle-knife is passed through
the opening in the lens.
|
LENSES USED IN LASER SURGERY Recently, a number of laser techniques for the treatment of open-angle
glaucoma have been devised that require clear visualization of the anterior
chamber angle and/or the ciliary processes. The procedure that has
received the greatest acceptance and that is used most widely is laser
trabeculoplasty. Another technique, goniophotocoagulation, involves
photocoagulation of neovascular vessels bridging the angle. Since these
laser procedures utilize a slit-lamp delivery system, one of the various
mirrored goniolenses must be used rather than a direct gonioscopy
lens. However, a number of modifications have been made in the standard
lenses to improve their usefulness in laser treatments. Special anti-reflective
coatings have been bonded onto the surface of the lens
to reduce the glare and scatter of the laser energy.3 Other lenses have had small high-plus buttons bonded onto their surface
over the mirrors to increase magnification of the structures being seen. Some
lenses have been constructed of different materials because
the glass or acrylic lenses available for general use cannot tolerate
the high energy impact of the short-duration pulsed lasers that are now
being employed with increased frequency. At least one manufacturer of
a neodymium: YAG laser provides two special mirrored gonioscopy lenses
with a 7-mm and 8-mm radius of curvature. These lenses are made of
special glass and are much heavier than the standard plastic lenses that
are used for diagnostic purposes. |