EVALUATION OF PEOPLE WITH LOW VISION
When evaluating patients with low vision the clinician must understand not only their visual problems but their psychological problems as well. In addition many of these patients, as they age, have other medical problems, which may include loss of hearing and arthritis. All these factors must be taken into account when dealing with their visual problems.
There are many psychosocial factors in vision rehabilitation given that loss of vision changes the course of one's life and alters relationships with many patients including family, friends, and coworkers. The ability to adapt to vision loss depends not only on the diagnosis and attendant visual problems but also on the patient's interaction with others. The age at which this vision loss occurs is crucial. If a loss of vision occurs when the patient is young and working it may mean a drastic change in the ability to carry on a career. If this loss occurs when the patient is older and retired, however, it affects relationships with spouses, children, and friends and often contributes to a loss of self-esteem. People with vision loss often experience a period of great sadness before adjustment occurs.
This grief process has been described as being divisible into six stages and is often compared with that of grieving a terminal illness.27 Past life must be left behind and the afflicted person must learn to grasp a new physical reality emotionally and intellectually. At first when patients learn what their problem is they are shocked and upset. This stage is then followed by denial, an unconscious response, which normally occurs to deal with the intense anxiety that ensues. Many patients at this stage may deny the seriousness of their conditions and also be noncompliant in caring for themselves. It is often difficult for the ophthalmologist to inform patients that their vision will not improve. In a study performed at the Massachusetts Eye and Ear Infirmary Vision Rehabilitation Center, 25% of all interviewed patients examined denied that they knew what was the matter with their eyes, claiming that no one told them,3 even though their cases had been discussed many times with them by their eye care specialists and low vision evaluators. Unless affected patients recognize their problem, it is impossible to achieve vision rehabilitation successfully. The ophthalmologist must not offer any hope for a cure for the problem but explain to the patient that she or he must learn now to use any residual vision. The next stage many encounter is that of guilt, that in some way they caused their vision loss. It is important to inform these patients about the problem, acknowledge their grief, and provide them with honest answers to their questions. The third stage is often one of bargaining in which patients may believe they may derive some benefit if the perform certain tasks, such as eating special foods and diets, taking vitamins, or contributing to charity as if this may somehow reverse the diagnosis. The fourth stage is anger, because such patients are often angry about why this problem should happen to them and why many others of their age do not have this problem. Many patients may be angry at their ophthalmologist for “creating” this problem. Many blame their ophthalmologist for shining a bright light in their eyes and then claiming that they could not see after that dilated retinal examination. At this stage, the clinician must explain to the patient as well as to family members that this vision loss is something that occurred and that they must learn to use their residual vision. The fifth stage is depression, which may be temporary or long term. This stage usually occurs when patients understand that their vision loss is permanent and major adjustments are necessary. Such afflicted patients should be counseled, supported, and encouraged to learn new skills and adaptive techniques. Many such patients may even become suicidal; it is important to be aware of this and make certain that this does not occur. The sixth and final stage is one of adaptation and hopefully this stage continues for a long time. During this phase, patients discuss their visual problems with increasing ease and develop realistic short and long-term plans. It is important to let them try to do whatever they would like to do with their eyes and work together with them and encourage use of the eyes.
Families should accompany patients during the examination so the family members can be part of the grieving and resolution of the various phases the patients are going through. Many family members also pass through these stages of grief experienced by those experiencing vision loss.
Vision rehabilitation can be performed in an office by an ophthalmologist, an optometrist, or with the aid of ophthalmic technicians.28 This is an area where ophthalmologists can work together with optometrists in a harmonious relationship. A more complex approach to a low vision evaluation, such as evaluating multiple vision aids, can be performed at a major center or at a large practice. This can be a facility for the visually impaired or at a medical center.29 Most patients would find it more convenient having their vision rehabilitation evaluation performed close to home but sometimes this is impossible.
If a practitioner intends to perform vision rehabilitation in the office, it is important to have some vision testing materials for distance and near. There could include a trial frame, lenses for refraction, an Amsler grid, and contrast sensitivity function tests and glare testing. It is often helpful to have a trial set of basic low vision optic aids along with some reading lamps and writing material. It is important when performing a vision rehabilitation evaluation to inquire what the patient would like to be able to accomplish visually. Most patients examined for vision rehabilitation wish to be able to read, including newspapers and magazines. Because many patients were not necessarily born in the United States, it is helpful to have reading materials in the patient's native language. This may include various foreign language newspapers or magazines (Fig. 1). It is often helpful to ask patients to bring in their own magazines or newspapers and test the vision with their own reading material. It is also helpful to have a reading stand and other samples of typical reading material such as the comics, crossword puzzles, obituaries, and the stock market page as well as playing cards and sewing materials.
THE EVALUATION
A visual rehabilitation examination should be considered only the first step in a process for those with irreversible vision loss. The objective of this evaluation is to enable patients with vision problems to maximize their residual vision through the use of adaptive devices and techniques.
The first stage in every evaluation is one of history taking. As the first stage in the taking of the history, it is important to ask patients why they have come for the evaluation. Many patients who have this type of evaluation often reply that they don't know. It is then important to educate the patient and family members why the examination is taking place. Most patients who are having this type of evaluation wish to be able to read and this is where vision rehabilitation is most helpful. After the primary visual motive is determined, it is important to ask the patient about other visual tasks and whether they are presenting any problems. It is important to inquire whether the patient can get around in a familiar or unfamiliar area. The familiar area can be inside the home or in a shopping mall. Many patients wish to maintain their financial independence and it is important to inquire whether they can write a check or a letter. Most patients wish to be able to read and it is important to find out what they would like to be able to read. Many patients wish to read television listings and unfortunately the print in most such material is very small and difficult for many of our patients to use. Most US patients like to watch television and it is important to inquire whether they have any difficulties in this area. Moreover, the clinician should encourage patients to sit as close as they would like to the television screen because the magnification of nearness is of great help to these patients. At the same time, the clinician should ask whether the patient likes to go to the movies and if so, does this present any problems. Many would like to be able to but have difficulty in the theater; so again, it is helpful to encourage these patients to sit in the front of the theater rather than in the back. The patient must be assured that sitting close to the television screen or the movie screen will not damage or injure their eyes in any way. Most restaurant menus usually have black print on a white background, which is the easiest contrast print for our patients to read. Unfortunately, a small percentage of restaurants may have menus with colors that offer poor contrast, such as black print on a red background, and for most this is very difficult to read. Many restaurants have dim illumination that makes it even more difficult for those with impaired vision to read menus. Some patients listen to whatever someone else is ordering and inform the waiter or waitress that they “will have the same thing.” Family members and friends should be encouraged to help visually impaired patients with their menu selections and, of course, the waiter or waitress can also describe many of the foods presented. When in a restaurant, family members may be helpful in orienting food on the plate and, in fact, some patients may need help in cutting meat into bite-sized portions. Patients should be asked whether they have any problem pouring liquids either at home or in the restaurant. Many patients at home have hot tea or coffee in the morning and it is important to instruct them in how to do this safely to prevent burning themselves or missing the cup. Some patients have hobbies, many collect coins or stamps, and it is important to encourage them to continue with whatever hobby they enjoy with the help of optic or nonoptic approaches.
ASSESSMENT OF VISION
Both near and distance visual acuity of all patients who have vision problems must be measured and evaluated accurately. For many patients, it is not possible to test at the usual distance of 20 ft. Testing of visual acuity can also be accomplished at a shorter distance. It is important to record the visual data as measured for near and far. These numbers can be converted to 20-ft Snellen designation by multiplying both the numerator and denominator of the visual acuity by the number that converts that numerator to 20. For example, the patient who reads the 20/40 line at 10 ft viewing the Snellen type can be recorded as having 10/40 or 20/80 (10/40 × 2/2 = 20/80) vision. This conversion to the 20-ft designation can be helpful when reports regarding these patients are sent to outside agencies. Outside agencies may not understand 10/40 and what this means but they will understand 20/80. It is also important to not only measure each patient's eye individually but with binocular vision. Quite often, binocularity improves the vision a sufficient amount that the patient can function well with conventional lenses rather than with special low vision devices.
Various charts are available that can be very helpful for vision testing. These include the BaileyLovie, the Bausch and Lomb, the Sloan letter chart, and the Early Treatment Diabetic Retinopathy Study (ETDRS) charts (Fig. 2). These charts are recommended because they are simple, accurate, and reproducible. Standard Snellen charts usually underestimate the acuity of patients who have vision between 20/80 and 20/200. The other advantage of testing patients closer to the charts than 20 ft is that the patient feels a sense of accomplishment knowing he or she is able to read several lines on a chart that may be 10 or 5 ft away. It is important to congratulate and encourage these patients during the examination as they read the lines.
|
Near visual acuity can be measured in several ways. There are some special reading charts with single letters modeled on the ETDRS distance chart, such as the Lighthouse Near Test card and quite often it is helpful to measure patients with whatever reading material they would like to be able to read (Fig. 3). This can be the patient's own magazines or newspapers and this makes much more sense to patients who wish to be able to read these very materials. The reading visual acuity score then can be recorded by measuring the size of the type on the page. Of course, these measurements should be conducted with the patient's own reading glasses or bifocals or with a correction recommended by the examiner.
|
Many low vision acuity charts differ from regular charts in several ways. Each line of optotype is an equal factor smaller than the previous line and each line contains optotypes with similar resolution difficulty. There is also a proportional decrease in spacing that is equal to letter width in each particular line. Of course, the ability to resolve optotypes visually does not directly correlate with the ability to read text, and that is why it is important for patients to be tested on their preferred reading material.
Some patients are not able to read letters because of unfamiliar language, illiteracy, or other types of cognitive impairment. For these patients, it is important to use number charts, symbol cards, or testing cards for the illiterate, which are available (Fig. 4). Even though some patients may be illiterate in reading letters, most can read numbers so that this is an important way of testing vision for near and far.
|
Another test that may be important to a visually impaired patient is the visual field.30,31 The clinician must know the location, density, size and the shape of central and peripheral visual field deficits to place reading material in an area where there is no visual field loss. Many patients with dense central scotomas, particularly those with macular degeneration, have difficulty with straight ahead vision and it is important to position the reading material to the right or left of fixation. Often the combination of performing a visual field test and vision rehabilitation examination on the same day may be too fatiguing for many elderly patients. Confrontation fields should be attempted because they are often very helpful. By knowing the area of the visual field loss, the low vision evaluator can best explain to the patient and family where to position materials to achieve the best possible vision. This also holds for distant vision but most patients quickly discover the head and eye position that provides maximum vision. This is very helpful for the patients who would like to walk around the neighborhood, watch television, and use their eyes for near, intermediate, and distance visual tasks.
Besides confrontation testing, several others means exist to measure visual field tests from the tangent screen to the Goldmann perimeter to the automatic visual field machines. The scanning laser ophthalmoscope (SLO) can also be used to plot the scotomas present and also find the preferred retinal locus for the best vision.32 In any case, whichever modality is chosen, best approach should include a relatively shorter time visual field test that is much easier for elderly patients to use.
Another possible visual measurement that may be important is that of color vision. Measuring color visual defects can be useful to many patients with loss of vision. For patients with severe vision loss, the Farnsworth D-15 color vision test can be used. This relatively inexpensive test can quickly be administered and can detect red, green, yellow, and blue perceptual defects.
Many partially sighted patients complain of an increase in glare sensitivity. Quite often, normal sunglasses are too dark or not dark enough. This sensitivity occurs when light entering the eye is scattered, reflected, and diffused by surfaces in the media. Patients then complain of headache, fatigue, ocular discomfort, or a burning sensation in their eyes. Usually, these symptoms can be alleviated by adjusting the levels of surrounding illumination. Glare can occur with corneal scarring, cataracts, maculopathy, and neuropathy, as well as vitreous opacities.
Several methods of testing glare sensitivity are used, such as a small penlight shone into an patient's eyes when he or she is trying to read or with the brightness acuity tester (BAT). With this device, visual acuity can be tested under low, medium, and high levels of glare.
Besides controlling the direct source of illumination, glare can be reduced by using antireflective coatings on the front and back surfaces of spectacles or by adding an ultraviolet-400 coating. It is important to ask patients about their problems with lighting as well as to test it. Glare disability may indicate dry eyes and it is important to examine the patient for this condition. Glare disability may be improved with standard dry eye treatment.
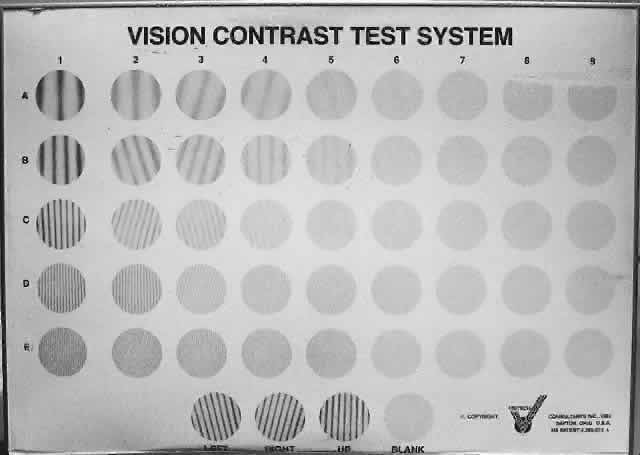
Contrast sensitivity testing may provide additional information, which can be used to measure a patient's ability to detect pattern stimuli at low-to-moderate contrast levels. A contrast sensitivity function test often gives a more complete designation of visual loss than visual acuity alone. The Vistech contrast sensitivity function screener, which can be used at 10 ft or modified to 3 ft, is available (Fig. 5).
|
REFRACTION
A careful refraction must represent part of a low vision examination. Quite often ordinary spectacles may be helpful and may be all that the patient with visual problems requires. It is best to perform a refraction with a trial frame and lens and use careful retinoscopy while the patient refracted views a nonaccommodative target. It is not advisable to use a refractor or phoropter for patients with visual acuities of less than 20/100 because it is often difficult to view through the small aperture lenses of this instrument eccentrically. It is much more practical for patients with low vision to have a trial frame refraction. The clinician should first aim for high accuracy with retinoscopy because the subjective evaluation is often difficult with visually impaired patients.
In performing a subjective examination of a patient with low vision, the patient should view the smallest optotypes that can be resolved with the objective refraction. The clinician then modifies the sphere by having the patient compare the manifest refraction with a + 0.50 diopter (D) sphere and then check with a -0.50 D sphere. If no difference is observed, a larger increment of changes such as a + /-1.00 D spheres can be used. The patient must maintain a view of the target from the point of fixation with each lens change. To ensure this, the examiner needs to make repeated short duration comparisons rather than allowing these patients time to refixate during lens changes. The cylindrical check can then be done either with a ±0.50 D handheld Jackson Cross cylinder (JCC) or if the patient is unable to resolve a difference in axis, power, or both a ±1.00 D handheld JCC can be substituted. Quite often patients with as little as 3/200 vision can differentiate increments of ±1.00 D sphere or cylinder while observing an object near their vision threshold. This measurement can be performed at the 5- or 10-ft distance given that such patients often are unable to view any chart at 20 ft.
After monocular refraction is completed for each eye, binocular acuity should be measured. Symptoms related to binocular vision should be explored at the trial frame stage. If symptomatic diplopia is present, prisms should be tried. For some patients with very poor vision in one eye, a clip-on opaque occluder may be necessary and helpful.
After completing the distance refraction, a near refraction is initiated. This is probably the most important part of any low vision refraction evaluation. The greatest amount of time spent in this evaluation is usually for near vision testing. A standard reading card can be used to test near vision at a conventional reading distance.
Many patients who also need increased magnification to read must be instructed how to hold the reading material closer to their eyes than they would ordinarily do. It is important to stress to patients, particularly elderly patients, that to achieve magnification, the reading material must be held closer, simultaneously reassuring them that this will not damage their eyes as they may have been told many years ago. Despite this assurance, many older patients will not hold reading material close to their eyes.
Various methods are available to measure near vision as well as recording near vision measurements. The M unit was introduced by Louise Sloan as a component in a method to determine the power of reading vision by having patients read print of graduated sizes at a distance of 40 cm.33 The smallest print is designated as 1.0 M because the overall dimensions of lower case letters subtend the visual angle at 5 minutes at a distance of 1 m. The series of sizes in M units runs from 1 to 10. The reading ability in M units multiplied by 2.5 is said to be equal to the power in diopters that will be required for the reading addition. For example, if a visually impaired patient is able to read only 10 M print at 40 cm, he or she will require a reading addition of 10× 2.5, or 25.00 D, to read ordinary newsprint or 1 M print. This reading power can be reduced if the patient has any accommodative power or if the patient is myopic. In elderly patients with cataracts, myopia often does increase and this aids the patient by affording some built-in magnification for nearness.
The Jaeger system was introduced more than 100 years ago and many records document near vision, using the Jaeger or J system. The only problem with this system is the size differences from one level of print to the next are neither uniform nor related mathematically.34 This system probably remains the most widely used today.
In 1866, Snellen devised a near vision test that is comparable with his distance test in that 5-minute overall angle exists in which each component of a letter comprises a 1-minute angle.35 Near vision is recorded as 14/14 or its equivalent 20/20. The metric system equivalence to 20/20 is 0.5 m or 6/6.
Another method is the point system, which is used in measurement of newspaper and book print. This system refers to the size of the type; the heights of the characters have a definite relationship to the type. “One-point” type measures 0.35 mm in height and “five-point” is 1.75 mm high. Publishers and typesetters of books and newspapers often refer to the point system. A decimal notation can also be used to describe the measurement of near visual acuity. In this system, vision is calculated by dividing the numerator of the Snellen fraction by its denominator. For example, 20/20 would be equivalent to 1.00 and 20/200 would be equivalent to 0.1. The decimal system is not usually used in the field of vision rehabilitation because it is awkward and is often difficult to compare with other measurements depending on the problems the patient has.
Often when performing a refraction, measurements are found to be somewhat similar to the patient's own spectacle prescription. In this case, a trial clip can be placed over the spectacle and lenses can be introduced into the trial clip for near testing. It is important when increasing magnification for near that the patient be instructed to hold the reading material closer to his or her face, and at the same time making certain that adequate light is available. As the reading material approaches close to the face, it is often difficult for light to fall on the page that is being viewed.
When refracting children with low vision problems, it is important to perform the manifest refraction and the reading evaluations before a cyclopegic refraction.36 It is necessary when performing a refraction to be as thorough and careful as possible; however, it should not be a lengthy examination because children tire quickly and become restless. It is wise to try to limit refraction duration to 10 minutes.
One approach to estimating the correct addition for reading is by calculating from the reciprocal of the Snellen visual acuity. Kestenbaum was the first to propose this method.37 His formula states that the diopter power of the reading for viewing Jaeger 5 type print is equal to the reciprocal of the distance visual acuity. In this situation, the denominator is divided by the numerator and the result is a predicted addition that would permit the patient to read ordinary print, which is generally ordinary magazine print. For example, if a patient has 20/200 vision, 200 ÷ 20 would be equal to 10 D of reading addition. If an patient has 10/200 vision, then the dioptric reading addition would be 20 D, which would be produced by dividing 200 by 10.
Telephone directory print is generally Jaeger 3 type print and the needed add for this is the reciprocal of the distance vision multiplied by 1.4. Therefore, a patient who requires 10 D of reading addition to read Jaeger 5 type or average newspaper print would need 14.00 D to read Jaeger 3 type (10 × 1.4 = 14.00 D).
If a change for reading prescription or for a bifocal is recommended, then the prescription should be placed in a trial frame and the patient given the opportunity to test the proposed glasses while reading a newspaper or magazine rather than the reading card. Any final adjustments can be made at this time.
For many low vision patients, changing only ordinary spectacles, either for distance or for near, is all that is necessary to ensure adequate vision rehabilitation. Many patients are used to spectacles and feel comfortable with them if improved vision can be obtained by this means.
In addition, other low vision devices can help those with severe visual defects. These fall into two main categories: optic devices and nonoptic devices. Optic devices (e.g., lenses, prisms, telescopes, or electronic devices) allow patients to see smaller, finer targets. Nonoptic devices improve visual function without the use of lenses.
OPTIC DEVICES
Telescopic Systems
The basic features of most telescopic systems are the separation of the objective and ocular lenses. Two basic types of telescopic systems exist. First, there is the Galilean telescope and second, there is the astronomic or Kepler telescope. The Galilean telescope consists of a convex objective lens and a concave ocular lens separated by a difference of their focal lens. Looking through this type of telescope, one sees an upright magnified virtual image.
The Kepler or astronomic telescope consists of two convex lenses separated by the sum of their focal lens. This system when viewed produces a magnified inverted image. To view upright, mirrors or prisms are needed to invert the image. Most binoculars have this type of telescope system. Because of the need for this prism, the application of the astronomic telescope for vision rehabilitation is limited because of the size and weight of the elements involved even though the magnification is often greater. The first telescopes, which were prescribed in the form of glasses, were prescribed in 1646; in 1667, a telescopic spectacle was prescribed for near for a patient with a myopia of -6.25 D.38 At the beginning of the 20th century, telescopes were developed, promoted, and used for visual rehabilitation; however, at that time, it was thought that patients with a great deal of nearsightedness should not wear full correction spectacles. In fact, clinicians believed that it was preferable to remove a clear crystalline lens from the eye to reduce myopia rather than use a device. When this surgery was performed at the beginning of the twentieth century, some disastrous results ensued. Recently, clear lens extraction for high myopia is being tried once again but the risk of postoperative retinal detachment remains significant. These days it is accepted that patients with high myopia can wear full correction spectacles. However, many patients consider that a full spectacle correction is harmful to the eyes and causes them to worsen; this, of course, is not true.
Telescopic systems have many limitations. Telescopic spectacles are associated with problems such as a reduction in the field of view, scotomas, parallax, decreased depth of focus, and a loss of light transmission as light passes through multiple lens surfaces. Telescopic spectacle systems are used by a limited number of patients on an intermittent basis where they are seated, for example, in outdoor stadiums watching sporting events or in the theater. Telescopic systems are useful when it is not possible to obtain adequate magnification by moving closer (Fig. 6). Telescopes may be handheld, mounted in spectacles, or placed on a stand. They can range in power from 1.7× to 20× magnification. Large spectacle-borne telescopes are suitable for sedentary distance viewing but handheld or ring style telescopes are more suitable for distance spotting such as street and bus signs, blackboards, wall menus, directories on buildings and directories on building walls. Some telescopic spectacles can be focused at intermediate distances for work at the computer or word processor. In the field of medicine, surgeons working in cardiovascular or hand surgery often use spectacles with telescopes with reading additions to allow them mobility and magnification without having to move too close to the surgical field. Ophthalmologists have also used these telescopic spectacles for ophthalmic surgery.
|
Driving with telescopic lenses has always been considered controversial.39 Many years ago the only way in which a person could pass a driver's test was to have spectacle- or contact lens-corrected 20/40 vision or better. Years before that, however, it was only 20/70. Most states in the United States have now modified their driving visual requirements in that 20/40 is the designated 24-hour driving vision and the 20/70 visual acuity needed to pass the driver's test for daylight driving only. Daylight driving is designated as 1 hour before sunrise and 1 hour after sunset. The reason telescopic lenses are considered controversial is because of the limited field, which reduces peripheral vision. Considerable training is necessary to achieve success with these generally expensive spectacles. Some practitioners who prescribe telescopic lenses for driving often prescribe the telescope to be placed at the top of the lens of one spectacle and recommend using it for spotting purposes only. Some patients use telescopic spectacles for watching television at a distance even though these lenses limit the depth of focus and the peripheral visual field. Having patients sit close to the television screen affords a wider field and the magnification of nearness.
Telescopes can also be used for near and intermediate tasks. One can focus telescopes for near viewing by adding plus lenses behind the ocular, by adding plus lenses in front of the objective lens, or finally by increasing the tube length of the telescope.
The greatest advantage of using a near focused telescope for a close visual task is the increased working distance afforded the user. The working distance with a near telescope is increased over a simple microscopic magnifying spectacle by a factor of the power of the telescope. For example, a 3× telemicroscopic system focuses at 10 in whereas a similar 3× microscopic spectacle focuses at 3.3 in. The disadvantages of this telescopic system, however, are reduced depth of focus and a smaller field of vision.
Several reasons suggest that the telemicroscopic or near focused telescopic systems are useful in tasks that prohibit close working distance and require the hands to be free (e.g., viewing computer monitors, reading music to play musical instruments, crafts, mechanical work, typing, drafting). These near focused telescopic systems are available as spectacle borne, spectacle mounted, handheld, or mounted on a tripod. There are also slip on, clip-on monocular telescopes that can be placed over spectacles for intermittent use such as in classroom lectures and then can be removed from the spectacle and slipped back into a pocket to carry easily. There are also some investigative intraocular implants being developed, which have a highly minus concave lens in the center of a convex intraocular lens implant. During routine activity, these patients may benefit from the normal power of the intraocular lens but when a strong convex spectacle is placed before their eyes another type of Galilean telescopic system is created. These implants may be used in the future for patients with macular degeneration who have difficulty with distance vision. These patients can presumably use this system while seated and looking out into the distance. These implants may also produce double vision. It is still open to question whether these intraocular lens implant telescopes are of help to those visually impaired.
CONTACT LENSES
Contact lenses are another optic device for use in vision rehabilitation. They are particularly useful in situations when irregular corneal refractive surfaces produce blurry vision such as in keratoconus and in some highly myopic states. Contact lens in these situation provide an enlarged, less distorted retinal image. Before the days of intraocular lens implantations, contact lenses were of enormous help to aphakic patients. Very few patients are left aphakic these days and those who are can wear contact lenses or have the secondary placement of intraocular lenses. There are also patients with no pupils in aniridia who would benefit from contact lenses with an opaque iris painted on it.
In a patient with binocular potential, it is helpful if a patient can us both eyes together in reading. This is possible in vision rehabilitation to a maximum binocular spectacle reading addition of + 4.00 to + 6.00 D. Many patients who are visually disabled may require this strong reading addition. However, with greater strength lenses, the focal length must be shorter. The greater the reading addition the closer the patient must hold the print to his or her eyes. Again, the clinician must stress to the patient that it is not harmful to hold reading material as close to the eyes as necessary.
The simplest type of spectacles for reading are single vision lenses. Many patients are accustomed to bifocals, and of course, these can be prescribed for close work. High plus reading bifocals or reading spectacles make it difficult to achieve binocular visual acuity unless significant prism or decentration is incorporated into the lenses to compensate for the amount of convergence required to read at close distances. A very helpful rule of thumb is the one that was devised by Gerald Fonda according to which he recommended decentering in each reading segment by 1 mm for each diopter of reading addition for each eye.40 If, for example, a + 5.00 D reading addition is recommended, each individual lens should be decentered in 5 mm. Most patients with severe low vision problems usually do not have binocular vision, but using binocular vision is attainable, it is definitely of benefit to these patients. In general, a + 6.00 D reading addition is the maximum that can be used to achieve binocular vision.41
Many different types of reading glasses exist; one of the most popular is half-eye glasses that are usually preferred because they are lighter lenses and patients can look over the top for distance vision. Testing sets of reading spectacles are available (Fig. 7). Some people prefer full-size single vision reading spectacles because the lenses provide a larger field but they must be removed for distance vision and may be heavy if the reading additions are strong. Bifocals are indicated if significant distant correction is necessary and high-powered trifocals may be prescribed, which allow patients to read smaller print more closely while permitting them to read larger print at an intermediate distance. Some patients, for example, would like to read the newspaper to read the death notices or stock market reports, which are in smaller print, which the reading addition allows the patient to see. Many determining factors influence the power of the reading addition, including the distant refractive measurements, patient age, type size, ocular pathology, and the degree of illumination used while reading.
|
Visually impaired patients sometimes have problems with high plus spectacle lenses in that spherical aberrations may be created unless aspheric lenses are prescribed. Another problem is difficulty in providing illumination on the reading material because the eye is positioned closer to the page. Patients must learn to hold reading material at the proper distance and, as discussed earlier, this is usually not so difficult with younger as with older patients.
Lens magnifications are rated. An arbitrary reference to lens magnification states that a + 4.00 D reading lens has 1× magnification and a + 8.00 D lens has 2× magnification. This general formula states the magnification equals the number of D divided by four. Therefore, a + 16.00 D lens would have 4× magnification. This formula, however, is not accurate because it is based on the assumption that the average reading distance is 25 cm. These calculations do provide a reference value for understanding how the optic manufacturers correlate dioptric and magnification units.
HANDHELD AND STAND MAGNIFIERS
Handheld and stand magnifiers are nonspectacle magnifiers. These are often very helpful to patients who have near vision problems. These convex lenses may be designed with a handle or a stand and are portable. The advantages of handheld magnifiers are that they are easy to use when viewing eccentrically and they are most useful for short-term tasks. They are also familiar to patients and usually inexpensive. These handheld and stand magnifiers can be used along with distance and reading spectacles or the bifocal reading addition. Some disadvantages of handheld magnifiers are reduced field of view compared with that provided by spectacles and the difficulty encountered in patients who have tremors. Handheld devices must be held at the correct focal distance to obtain maximum power. Handheld magnifiers are available in a wide range of powers, size, and shape from + 3.00 D to 20× magnification. Some handheld magnifiers also have their own internal illumination source (Fig. 8). Stand magnifiers are composed of a convex lens attached to a stand that holds it at a fixed distance from the page. They are available as either fixed focus or focusable models. A virtual image is formed a short distance behind the lens (Fig. 9). Patients who use stand magnifiers must supply some accommodation or wear convex lenses to focus the emerging divergent light rays. The advantage of this type of magnifier is that this lens is stable because it is resting on a surface, and the object is always in focus because the object-lens distance is thereby fixed. The disadvantages of this system, as is the situation with handheld magnifiers, are that the field of vision is small and it is difficult to use unless the surfaces are flat. The lens in the focusable stand magnifier is adjustable.
|
Another type of stand magnifier is the Visolette (see Fig. 9). This model has a constant magnification of approximately 1.8× to 2.2× and concentrates the light diffusely on the object with a minimal peripheral distortion. This is an advantage if the patient's head blocks some of the ambient light. This magnifier can be used with a spectacle magnifier and is useful for patients with tremors or poor hand coordination because it rests on the page.
ELECTRONIC MAGNIFIERS
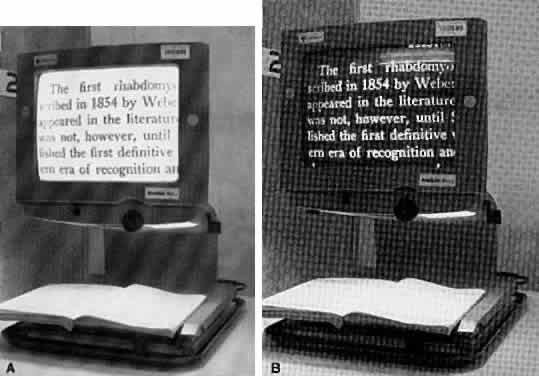
Closed circuit television (CCTV) magnifiers often provide excellent contrast and magnification; they can also furnish color and reverse contrast polarity (Fig. 10). Many patients can read with these devices. The print is projected white on a black background, advantageous because the projected black page reduces glare. These devices can provide linear magnification electronically up to 60× . This device can be modified for various uses in reading, writing, typing, crafts, computers, blackboards, and other sedentary distance viewing activities. An evaluation with a CCTV magnifier is important for patients who have high reading demands or severe visual field loss or those who require 6× or more magnification for near. The limitations of the use of CCTVs are that they may be expensive, heavy, scarcely portable, and may be difficult for some people to use. Many public and university libraries have these electronic devices. Some newer devices connect to television sets and can be used for near and far. Other headborne devices electronically magnify for distance and for near. These may be suitable for some patients but others find it difficult to wear them for extended period of time.
PATHOLOGY AND VISION REHABILITATION
Pathology of the eye or brain can cause several categories of visual defects.42 First, there can be an overall general field defect with diffuse, blurry, hazy vision; second, a central visual field defect, and third, a peripheral field defect. Some patients may have a combination of all or some of these visual problems. Patients with central blurry vision often have central distortion and a scotoma in the central fields, which can originate at or near the macular region. Those with peripheral field problems have loss of portions of the peripheral field with constriction of field.
Age-related maculopathy, cataract, glaucoma, and diabetic retinopathy are the main causes of loss of vision in developed countries.43–47 This has also been true in studies performed in the past in the Vision Rehabilitation Center of the Massachusetts Eye and Ear Infirmary.48
Adult cataracts as well as cataracts in children are an increasingly creating general central and peripheral visual problems: it is estimated that more than 50 million people are affected worldwide.49 These people have symptoms of blurred vision, poor contrast, glare, photophobia, faulty color perception, and often have difficulty reading and driving because of their cataracts. Ophthalmologic and biomicroscopic examination identifies the type of cataract so that diagnosis is often easy. The possible risk factors for cataract formation include diet, antioxidants, alcohol intake, sun exposure, diabetes mellitus, galactosemia, and severe diarrhea.50 It is important in all patients with cataracts that the retina should also be carefully examined to rule out any macular disease. Cataract extraction can benefit these patients even though macular pathology may be present. There should be a realistic discussion with the patient as to the potential for visual improvement. Cataract surgery is one of the commonest surgical procedures performed in the United States.51 Many patients with immature cataracts are served best by having a very careful refraction and given the best possible spectacle correction. Cataract surgery, as with any surgery, has both risks and benefits and although the benefits far outweigh the risks, a change of glasses is often the best first approach to the patient with immature cataracts that do not interfere significantly with visual function. These days with modern cataract surgery and with the implantation of intraocular lenses, restoration of vision is usually quickly and safely accomplished.
Macular disease, particularly age-related macular degeneration, is one of the leading causes of visual impairment in our society. Affected patients may have atrophy, fibrovascular scarring, pigment clumping, hemorrhage, or localized cystic changes in the macula and perimacular regions. There are great variations in the development of this maculopathy; many patients with advanced degenerative signs often may have good vision yet other patients who do not appear to have very much retinal damage may have severe visual impairment. It is important in evaluating these patients that all modalities of investigation be performed to provide the best care. All such patients should have potential acuity evaluations to ascertain their best possible vision. Other testing procedures that may provide valuable information include visual field testing and scanning laser ophthalmoscopy. These patients have central scotomas so that it is important to document the depth and position of the scotoma to use the peripheral intact retinal areas in the visual rehabilitation process.
Glaucoma is a dominant cause of visual loss. Generally, patients with this condition have a peripheral visual field loss that may ultimately lead to central field loss. It has been estimated that glaucoma is the second leading cause of bilateral blindness in the world.52 It is also a disease that goes undetected in its early stages. For these reasons, suspect patients must have accurate visual field studies made to determine where visual field losses and scotomas exist. Many glaucoma patients also have cataracts. Some may benefit from removal of the cataract and implantation of an intraocular lens accompanied by a glaucoma filtration procedure. In the past, the only eyedrops that were available for glaucoma were miotics, which made the pupil very small and often created visual problems. Today, many more topical medications are available to treat glaucoma as well as therapy using argon laser trabeculoplasty. Glaucoma patients must repeat the visual field test periodically to ascertain that the disease is truly under control as well as to protect their vision rehabilitation status.
Diabetic retinopathy is an increasing problem in contemporary civilization and is the leading cause of blindness in the United States in people between the ages of 20 to 74 years.53 Frequently patients with diabetic retinopathy present with variable visual acuity, distortion, and floating spots. Patients with diabetic retinopathy are also afflicted affiliated with other complications of diabetes mellitus such as diabetic neuropathy, strokes, and renal, circulatory, and coronary artery diseases. These complications may place an added burden and importance on the vision rehabilitation.
Patients with diabetes frequently complain about fluctuating vision. For this reason, it may be useful to test refraction in labile patients with diabetes on more than one occasion before prescribing spectacles. Diabetic retinopathy is related to both duration of disease and control of blood sugar. Patients with diabetes should be encouraged to monitor blood sugar levels, exercise, watch the diet, and pay particular attention to the prescribed medication schedule. Management of diabetes is a lifelong process and these affected patients must take responsibility for caring for themselves forever. The vision rehabilitation team can provide valuable support and encouragement.
CHANGES RELATED TO AGING
Many normal and pathologic changes occur with aging.54 With maturity, accommodation relaxes and progressively stronger reading spectacles are necessary. Those who are visually impaired may need higher-powered convex lenses along with some nonoptic aids to read. With aging, growth and yellowing of the crystalline lens reduces the amount of light entering the eye and thus more light is needed to read comfortably. Elderly patients often complain of glare and discomfort when reading indicating that they need to remember to blink and periodically look away from their newspapers or magazines. Along with the growth of cataracts, older people often develop dry eyes. This can occur with age, be secondary to medication, or be part of Sjögren's syndrome. Ocular lubricants such as artificial tears often relieve this condition greatly.
Many people have a type of phoria; as they age some have greater difficulty maintaining binocular vision. Ocular muscle paresis may develop secondary to an intracranial ischemic process resulting in debilitating diplopia. Prism correction incorporated into the spectacles may provide a functional miracle for many such patients. With aging, the pupil tends to become smaller and more light is needed for reading. Patients must be advised to use a lamp with an incandescent yellow light for more comfortable reading.
Many elderly patients these days are becoming more computer literate and the use of computers can be very demanding visually. Patients should be encouraged to increase blinking, look away, use lubricating eyedrops, and periodically rest their eyes when they are using video display terminals. It is important to explain to patients that their reading glasses or bifocals may not be the proper power because the video terminal is farther away than the ordinary reading distance. A special lens focused at the computer screen distance is helpful. Computer technology assistance is available to the visually impaired that uses enhanced contrast, magnification, and improved screen resolution.55 These devices increase the expense of a computer system, but they can be helpful for the well-motivated patient.
VISION REHABILITATION IN CHILDREN
Estimates suggest totals of more than 1 million blind children in the world with an additional 200,000 who cannot see because of cataracts.56–58 Children can be victims of diseases of the eye and central nervous system as well as accidents that cause partial or total loss of vision.59 Retinopathy of prematurity increases in children because oxygen is given more often to premature infants to ensure their survival. Such children should be monitored carefully and their retinas examined frequently. All pediatricians should carefully examine infants to rule out ocular disease and seek retinal consultation if there are suspected problems.
The examining eye physician should be aware that many children with visual problems may also have hearing disorders. In deaf children, 35% have some type of attendant ocular problem that interferes with good vision, including refractive anomalies and ocular pathologies.60 This compares with about 10% of children with normal hearing. In deaf children, 75% become so at birth secondary to perinatal problems, genetic mutations, inheritance, and unknown factors.61 The other 25% of deaf children are considered postnatally deaf secondary to early childhood illnesses, cognitive genetic disorders, chronic serous otitis media, and unknown factors. The most common ophthalmic conditions associated with deafness in children are rubella retinopathy,, retinitis pigmentosa, and Usher's, Waardenburg's, Konigmark's, and Mobius's syndromes. The presence of deafness in a child places added emphasis on vision rehabilitation.
SUPPORTIVE PERSONNEL
Visual rehabilitation cannot be achieved only with optic approaches; other medical professionals may also offer great help in the rehabilitation of the visually impaired. These include occupational therapists, social workers, and orientation and mobility instructors.
Occupational therapy is an important part of the vision rehabilitation process,62 which helps people achieve their desire for functional independence through therapeutic use of activities that are important to them. Occupational therapists are available in hospitals, as well as on an outpatient basis. They can help the visually disabled by visiting their homes and offices and providing instruction in adaptive techniques and use of optic devices, as well as in coordinating self care, work, and recreational activities. Occupational therapists help to determine whether the optic devices prescribed meet the patient's task-specific needs. Patients may experience difficulty using optic devices because of arthritis, physical handicaps or motivational attitudes. An occupational therapist can adapt the device to make it easier to grasp by working with the patient. An occupational therapist may also substitute another magnifier of equal power that may be easier to hold. If patients have difficulty changing the batteries in devices powered by them, the occupational therapist can be helpful in this area. The therapist works with the client, shows the proper working distance and the use of devices, and provides instruction using verbal communications and visual or tactile demonstrations. The therapist modifies the teaching to the patient's level of understanding, cognitive status, and individual needs.
Social service is another profession that is helpful in working with visually disabled people.27 Social workers are available in both inpatient and outpatient settings. Usually the social worker assesses the patient after the patient has already been examined by both the low vision specialist and the occupational therapist. Psychological problems often accompany loss of vision. Grief, sadness, and denial are normal psychological reactions to vision loss. A social worker helps clients and their families work through these stages of sadness, grief, denial, and depression to achieve a state of acceptance of the present visual status. This is often a long process and social workers are often successful in this area. Some such may also need psychotherapy. In addition, social workers can direct communication with state agencies and other appropriate community resources. Social service is also available for financial resource referral areas and provide feedback to the examining optometrist, ophthalmologist, and occupational therapist about the patient's family situation and which needs are or are not being met and which local or state agencies may be of help to these patients.
Orientation-and-mobility instructors are available to train people with vision loss how to walk independently with safety and confidence. Such instructors train those with visual and other physical limitations to get around safely within their homes, their neighborhoods, their workplaces, and their communities. These training techniques include those with a sighted guide, indoor and outdoor travel (sometimes with a cane), auditory localization, safe street-corner crossing, and use of public transportation (e.g., buses, subways, taxis). Some patients may benefit from using a guide dog so that the orientation-and-mobility instructor can refer them to the proper organization to arrange this.
EVALUATION OF VISUAL FUNCTION
Ophthalmologists are often asked to evaluate permanent visual impairment and to relate it to the patient's permanent impairment. This is based on evaluation of three functions; corrected visual acuity, visual field studies, and ocular motility with diplopia. The equipment needed to provide this information includes visual acuity test charts, visual field equipment, a phoropter or retinoscope, and prisms. The historic standard for testing visual fields is the traditional stimulus III-4e of the Goldmann perimeter. Equivalent stimuli also can be produced with the Allergan-Humphrey Field Analyzer Perimeter (static, size 3) 10 decibels (algorithmic unit) or with the Octopus (static, size 3) 7 decibels (algorithmic unit) for phakic eyes. Published tables are available with visual acuity notations for distance and near with corresponding percentages of loss of central vision, loss in percentage of central vision in a single eye, loss of monocular visual field, and impairment of the visual system as it relates to overall impairment of the patient.63
In our mobile society, driving has always been controversial in association with those who are visually or physically impaired.64 It is estimated that 90% of the information input used for driving is visual.65 In the past, most states had a corrected visual acuity of 20/70 as acceptable for driving safely. Later, this was changed to 20/40. At present, 20/40 is the generally accepted best vision for 24-hour driving and 20/70 for daylight-restricted driving. Safe automobile driving is related not only to visual acuity and visual field but also to mental stability, ocular motor functions, neurologic function and stability, and intercurrent use of certain medications. In most US states, applicants need pass only a vision check to qualify physically for a driver's license. It has been shown that the accident rate for drivers older than 85 years is 2–3% greater than that of drivers between 45 and 50 years of age.68 Many people with impaired vision want to continue to drive. There are no absolutes in the area of the visually disabled and driving but there are guidelines and legal mandates regarding who may and who may not drive. Ophthalmologists cannot make the final decisions regarding a driver's license. States should provide road testing for the visually impaired and ophthalmologists should be members of the state advisory boards for driving.
Vision rehabilitation is an important goal that should be encouraged by all ophthalmologists. Millions of in the United States and millions more in other countries around the world suffer from low vision for which visual rehabilitation is available. All those with irreversible vision loss should have the opportunity to use their residual vision.
One of the great problems with low vision is that so many ophthalmologists do not inform their patients that the field of vision rehabilitation exists. In this era of innovative microsurgery and laser surgery, many ophthalmologists do not want to acknowledge to themselves that patients may be losing their vision and that no further surgery would be helpful to these patients. Ophthalmologists should not advise patients that “nothing more can be done.” All ophthalmologists must support their partially sighted patients by providing vision rehabilitation services or by referring them to services available elsewhere. It is important that all ophthalmology training programs educate their residents in low vision evaluation and vision rehabilitation. Orthopedic surgery, rheumatology, and cardiovascular training programs have rehabilitation programs, as does ophthalmology. The American Academy of Ophthalmology must expand its efforts with programs to increase the study and awareness of vision rehabilitation. Departments of ophthalmology nationwide must encourage not only the teaching of this specialty but also foster clinical research in this field, not only in the areas of optic and nonoptic approaches to vision rehabilitation but also in the realm of psychosocial factors associated with low vision.
Many eye care professionals believe that the low vision evaluation is too lengthy, nonproductive, and involves complex optic approaches. This is not true and much of the evaluation involves common sense. The optics of vision rehabilitation are not complex and it is possible to prescribe an optic or nonoptic approach reasonably quickly. It is helpful to have other clinical professionals available to assist with this evaluation (opticians, technicians, occupational therapists). Many patients with low vision are sad, angry, and depressed. There are professionals available to address for these psychological problems.
Vision rehabilitation has been shown to improve the quality of life of low vision patients markedly; affected patients have a high degree of satisfaction with this help.69 During the past decade, there have been remarkable achievements and accomplishments in better understanding of low vision and how to address it with a multidisciplinary approach.70 With continued commitment from eye care professionals, academic institutions, governmental agencies, and research facilities, further strides can be made in improving the function and quality of life for those with low vision, through the discipline of vision rehabilitation.