GENERAL Since their introduction to the U.S. market in the 1960s,3 PALs have steadily increased their share of the multifocal market. Several
studies have shown a large percentage of patients prefer PALs compared
to bifocal lenses.4–6 PALs provide a continuous change of power from distance through intermediate
to near that provides the wearer with a seamless visual space and
eliminates the unusable area of visual space caused by the top line
of a bifocal segment. A detracting feature of PALs is that the design
necessarily results in unwanted astigmatism in the periphery of the lens, usually
located in the lower diagonals relative to lens center. PALs have both cosmetic and vision advantages compared to segmented multifocals. The
cosmetic benefit results from the seamless design and is
apparent. The vision advantage results from elimination of the bisecting
region of unusable vision associated with the top of the bifocal segment, resulting
in contiguous visual space from distance through intermediate
to near. The vision advantage with PALs compared to bifocals
is supported by a study that showed patient preference for PALs compared
to a blended bifocal,7 both of which are seamless. The strong preference for PALs compared to
bifocals is further supported by another study8 in which 265 habitual bifocal wearers were fitted with PALs: 92% of
these patients preferred the PALs. Because progressive lenses have
no image jump and no areas of intermediate blur, many wearers describe
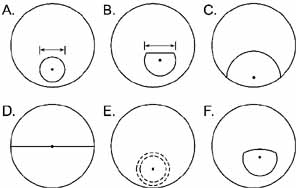
their vision with progressive lenses as more natural than with bifocals. OPTICAL CHARACTERISTICS Progressive addition lenses are designed to provide distance viewing in
straight-ahead gaze, a gradual progression of power in an intermediate
corridor, and the full addition power lower in the lens. The
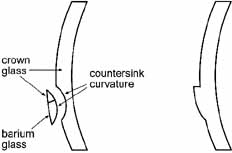
power change is accomplished by increasing the curvature of the front
surface (i.e., decreasing the radius of curvature) along the
corridor toward the bottom of the lens. Because the add must be spherical
in nature, the curvature must increase equally in all meridians (i.e., it
must increase in the horizontal as well as the vertical
meridian). As result, the horizontal curvature is flatter in the
upper portion of the lens and steeper in the lower portion of the lens. To
reconcile the curvature disparity and to make a seamless lens, surface
curvature must be altered in the lower quadrants of the lens. This
results in the unwanted astigmatism. Therefore, a necessary and undesirable
side effect of the gradual progression of power is unwanted astigmatism
in the periphery of the lens. The pattern of unwanted astigmatism
is a defining characteristic of individual PAL designs. The unwanted astigmatism limits the error-free viewing zones of
the PAL, resulting in considerably narrower error-free distance, intermediate, and
near-fixation fields than typical bifocal lenses. The
magnitude and location of unwanted astigmatism are worse with
higher adds (greater change in curvature required) and when
the distance and near centers are closer to one another (curvature
must change over a shorter distance). Primarily as a result
of the latter, the near zone of a PAL is lower in the lens than for a
FT bifocal. Whereas a very wide near zone is attained with a FT bifocal
with approximately 16 to 20 degrees of ocular depression, most PALs
require gaze depression of 30 to 35 degrees to obtain the near zone, one
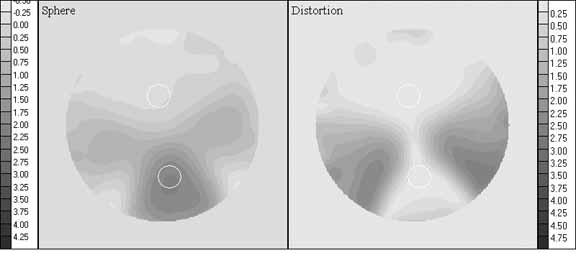
that is also considerably narrower than provided by a FT bifocal. A common method to represent the optics of PALs is with contour plots of
the spherical equivalent and unwanted astigmatism powers as shown in Figures 4 and 5. Because of the complex nature of the optics there are literally an infinite
number of possible PAL designs and dozens of different designs
are currently available. Although most current PALs defy clear categorization, it
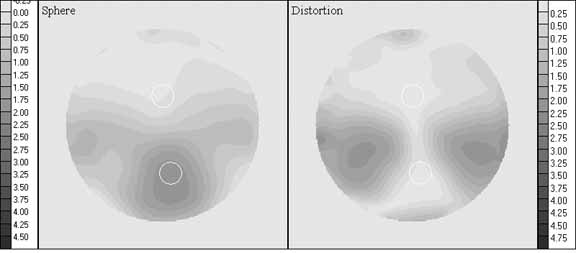
is instructive to consider the differences between a “hard” and “soft” design. The lens in Figure 4 shows characteristics of a hard design. Relatively speaking, a lens of
hard design has wider error-free distance and near-viewing
zones, the area of the lens with unwanted astigmatism is relatively
small, and the magnitude of the unwanted astigmatism is large. The separation
between the distance and near centers is shorter and the rate
of power change along the corridor is greater. The lens in Figure 5 shows soft design characteristics: narrower error-free distance
and near-viewing areas, larger area of unwanted astigmatism but
of lower magnitude, distance and near centers are farther apart, and
a lower rate of power change in the corridor. 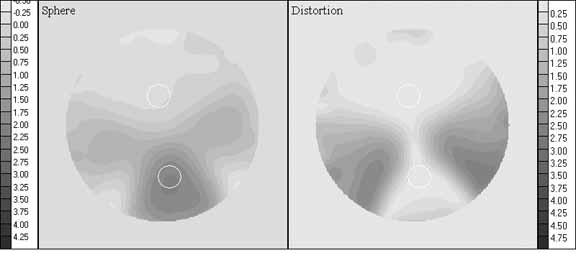 Fig. 4 Contour plots of spherical equivalent power (left) and unwanted astigmatism (right) for SOLA VIP, plano distance power, +2.00 D add. Contours in 0.25 D
steps. Fig. 4 Contour plots of spherical equivalent power (left) and unwanted astigmatism (right) for SOLA VIP, plano distance power, +2.00 D add. Contours in 0.25 D
steps.
|
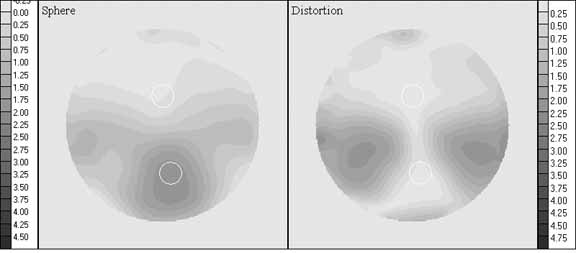 Fig. 5 Contour plots of spherical equivalent power (left) and unwanted astigmatism (right) for Varilux Comfort, plano distance power, +2.00 D add. Contours
in 0.25 D steps. Fig. 5 Contour plots of spherical equivalent power (left) and unwanted astigmatism (right) for Varilux Comfort, plano distance power, +2.00 D add. Contours
in 0.25 D steps.
|
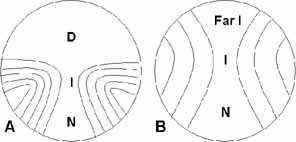
To accommodate the convergence that occurs with viewing at closer distances, the
central power corridor is nasally angled toward the bottom of
the lens to accommodate ocular convergence at near-viewing distances. Older
PAL designs used the same lens for right and left lenses
but angled in opposite directions. This approach resulted in the pattern
of zone widths and unwanted astigmatism being different to the two
eyes. Most current PALs use different lenses for right and left (essentially
mirror images of one another) in order to present the
same optical characteristics to each eye. The width and area of the error-free distance, intermediate, and
near viewing as well as the magnitude and distribution of unwanted astigmatism
can vary significantly across lens designs.9,10 There is considerable interdependence of the sizes and locations of the
viewing zones and the magnitude of unwanted astigmatism that make it
currently impossible to design a lens that is optimized for all optical
attributes. Hence, a particular PAL design may optimize one viewing
zone or characteristic, but it is at the expense of the other zones or
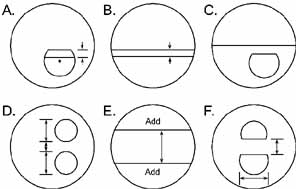
characteristics. The widths and areas of the three viewing zones (distance, intermediate, and
near) and the magnitude of unwanted astigmatism have been
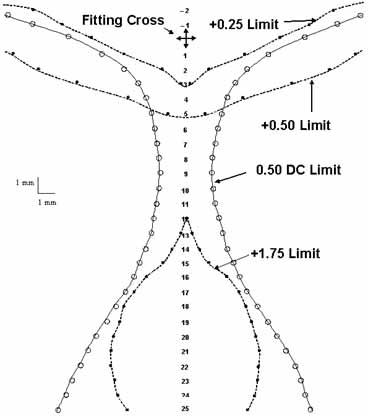
reported.11 The mean measurements are shown graphically in Figure 6. Analysis showed that even the largest intermediate and near error-free
zones are smaller than those required to view a typical computer
screen or standard paper respectively,11 and also smaller than the normal amount of ocular rotation used to view
noncentral targets.12 This means that the PAL wearer must learn to move their head more and
their eyes less in viewing noncentral objects and/or tolerate some
blurof typical noncentral foveally fixated objects. It is most likely
that the head and eye movement patterns are altered by PAL wearers,13 but the high acceptance and preference rates for PALs also indicate that
patients fairly readily are able to do so. 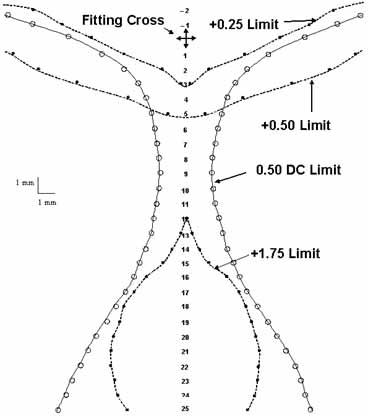 Fig. 6 Mean contours of 28 progressive addition lenses with nominal add of +2.00; data
acquired in 1-mm vertical steps. Contour for +1.75 add
shown because of greater consistency across lenses. For conversion
to visual fixation through the lens, 1 mm is approximately 2 degrees
of eye rotation. Fig. 6 Mean contours of 28 progressive addition lenses with nominal add of +2.00; data
acquired in 1-mm vertical steps. Contour for +1.75 add
shown because of greater consistency across lenses. For conversion
to visual fixation through the lens, 1 mm is approximately 2 degrees
of eye rotation.
|
PRESCRIBING PROGRESSIVE ADDITION LENSES For most patients a PAL satisfies general vision needs better than a segmented
bifocal. PALs should be considered a first option for general
visual use, unless cost is a consideration or the patient has specific
occupational or other visual needs that require the wider error-free
fields provided by segmented bifocals. Current successful bifocal or trifocal wearers will remain successful with
same lens design, although they would likely prefer the advantages
of a PAL. A large percentage of successful bifocal wearers prefer a PAL
if given the choice,8 although there is some risk in making the change. Determine if the bifocal-wearing
patient has specific occupational or other vision
needs that preclude recommending change to a PAL. Otherwise, the patient
can be advised of the vision and cosmetic differences between the lens
types in order to decide upon a possible change. For a first-time PAL wearer, selection of the particular PAL design
should consider the patient's specific visual needs. If a patient
is successfully wearing a particular design of PAL, they will likely continue
to be successful with the same design. However, consideration
should be given to a different PAL design if it better meets their specific
visual needs. As a direct result of the trade-offs in PAL design and the fact
that the various designs utilize different trade-offs, some PALs
can be expected to provide better vision at distance, intermediate, near
or various combinations of those distances. Ratings of 28 PAL designs
based upon the widths and areas of the distance, intermediate and
near-viewing zones and also the magnitude of unwanted astigmatism
are presented in Tables 3 to 7.11 These tables identify those lenses that can best meet the specific visual
needs of particular patients. Just as there is a range of optical
characteristics among PALs, there is also a range of visual needs among
patients. The clinical task is to match the two. Table 3 shows lens ratings along the single attributes of distance zone, intermediate
zone, and astigmatism. These ratings are useful for those patients
for whom there is a single over-riding need for one of those
attributes. For example, the distance rankings are used for patients
who drive a lot or are involved in outdoor work and have only occasional
need for intermediate and near vision. The intermediate rankings
are used for patients who want a general purpose PAL but whose primary
need is viewing a computer or performing a manufacturing task at intermediate
viewing distances. However, such patients may benefit even more
from an occupational progressive lens (see section on occupational
progressive lenses [OPLs]). The rankings based on
astigmatism are used for those patients who are very sensitive to unwanted
astigmatism and for whom this is the most important lens attribute.
TABLE 3. Calculated ratings for the distance zone, intermediate
zone, and unwanted astigmatism.
| Specialty usage—calculated ratings |
| Distance | Rating | Intermediate | Rating | Astigmatism | Rating |
| SOLA Percepta | 88.1 | Zei Gradal Top | 91.3 | J&J Definity | 93.3 |
| Younger Image | 87.4 | J&J Definity | 91.1 | Varlx Panamic | 70.0 |
| Shamr Genesis | 83.6 | Pentx AF Mini | 87.2 | AO Pro 15 | 69.3 |
| Ess Spr No-lne | 83.2 | Sig Nav Precsn | 84.6 | AO Compact | 66.7 |
| Vis Ease Outlk | 77.2 | AO Pro 15 | 84.6 | Rdnstk Life AT | 66.0 |
| AO b'Active | 69.3 | HoyaLux ECP | 83.6 | Pentx AF Mini | 61.3 |
| Sig Kodak | 67.1 | Rdnstk Life AT | 82.7 | Pentx AF 150 | 61.3 |
| Zei Gradal Top | 65.4 | SOLAMax | 76.7 | AO b'Active | 60.7 |
| Ess Natural | 54.6 | AO b'Active | 74.8 | Sig Kod Precise | 60.7 |
| J&J Definity | 53.0 | Sig Kodak | 71.0 | SOLAMax | 59.3 |
| SOLA VIP | 47.9 | Hoya Sum CD | 70.0 | Shamr Genesis | 55.3 |
| Rdnstk Life XS | 47.8 | Ess Adaptar | 62.0 | Younger Image | 54.0 |
| HoyaLux ECP | 47.4 | SOLA XL | 61.7 | Shamr Piccolo | 54.0 |
| Pentx AF 150 | 43.5 | Younger Image | 61.0 | Ess Adaptar | 48.0 |
| Varlx Panamic | 39.3 | Ess Natural | 60.8 | Hoya Sum CD | 47.3 |
| Sig Kod Precise | 37.3 | Varlx Panamic | 60.2 | Rdnstk Life XS | 46.7 |
| AO Pro 15 | 36.4 | Pentx AF 150 | 59.1 | Sig Kodak | 43.3 |
| Ess Adaptar | 35.3 | Shamr Genesis | 58.9 | Vis Ease Outlk | 42.0 |
| Varlx Comfort | 34.7 | Hoya GP Wide | 57.8 | Varlx Comfort | 39.3 |
| Hoya Sum CD | 30.1 | Varlx Comfort | 45.4 | Ess Natural | 38.7 |
| Sig Nav Precsn | 29.1 | Vis Ease Outlk | 44.0 | Hoya GP Wide | 38.0 |
| SOLA XL | 24.9 | Shamr Piccolo | 43.2 | Zei Gradal Top | 37.3 |
| Hoya GP Wide | 24.5 | Sig Kod Precise | 42.3 | HoyaLux ECP | 35.3 |
| AO Compact | 23.6 | SOLA VIP | 35.9 | SOLA XL | 31.3 |
| Shamr Piccolo | 23.1 | AO Compact | 31.9 | Sig Nav Precsn | 30.0 |
| Rdnstk Life AT | 17.6 | SOLA Percepta | 30.7 | SOLA Percepta | 30.0 |
| Pentx AF Mini | 16.2 | Rdnstk Life XS | 27.6 | SOLA VIP | 8.0 |
| SOLAMax | 7.1 | Ess Spr No-lne | 10.8 | Ess Spr No-lne | -29.3 |
Higher ratings indicate larger and wider areas of vision and lower astigmatism
magnitude. These ratings are useful for patients with a single
over riding need for distance vision, intermediate vision, or reduction
of unwanted astigmatism. (Reprinted with permission of Optometry.)
Table 4 shows ratings based only on the near-viewing zone. These ratings
are useful for those patients for whom near vision is the single overriding
need. This includes patients who perform extensive near tasks
yet also desire a general purpose PAL. It also includes emmetropic patients
who intend to use the lenses primarily as reading glasses but also
desire a general purpose PAL. An OPL should be considered for these
patients. The near ratings in Table 4 are directly derived from width and area magnitudes. As result, the ratings
generally increase with greater fitting height because a greater
fitting height necessarily results in a larger near-viewing zone
for all lenses. The larger ratings for greater fitting heights represent
the fact that the patient will have a larger and wider near-viewing
zone with a greater fitting height. Only a few lenses provide
any near addition for a fitting height of 16 mm. Note also that the
lens rankings change somewhat as a function of the fitting height. This
is because the manner in which the near zone changes toward the bottom
of the lens is different for the various lenses
TABLE 4. Calculated ratings for near zone
| Near specialty use—calculated ratings |
| Fit height 16 | Rating | Fit height 18 | Rating | Fit height 22 | Rating | Fit height 26 | Rating |
| Shamr Piccolo | 28.0 | Shamr Piccolo | 45.1 | Shamr Piccolo | 76.8 | SOLA VIP | 111.3 |
| Rdnstk Life XS | 27.2 | AO Compact | 41.1 | SOLA VIP | 76.2 | SOLAMax | 106.9 |
| AO Compact | 24.0 | Rdnstk Life XS | 40.2 | SOLAMax | 74.0 | Shamr Piccolo | 103.8 |
| SOLA VIP | 22.5 | SOLA VIP | 38.8 | Rdnstk Life XS | 71.9 | Rdnstk Life XS | 102.9 |
| Hoya Sum CD | 17.1 | SOLAMax | 38.3 | AO Compact | 65.9 | Hoya GP Wide | 98.3 |
| SOLAMax | 16.3 | Vis Ease Outlk | 30.4 | Ess Spr No-lne | 63.3 | Ess Spr No-lne | 80.1 |
| Sig Kod Precise | 14.8 | Ess Spr No-lne | 29.8 | Hoya GP Wide | 59.2 | Hoya Sum CD | 80.1 |
| Vis Ease Outlk | 13.0 | Sig Kod Precise | 28.6 | Sig Kod Precise | 57.3 | Varlx Comfort | 80.1 |
| Hoya GP Wide | 3.4 | Varlx Comfort | 26.6 | Varlx Comfort | 56.9 | HoyaLux ECP | 78.1 |
| J&J Definity | 0.0 | Shamr Genesis | 25.7 | Shamr Genesis | 54.2 | Sig Nav Precsn | 77.2 |
| Varlx Panamic | 0.0 | Hoya Sum CD | 23.2 | Sig Nav Precsn | 52.0 | Sig Kod Precise | 74.4 |
| AO Pro 15 | 0.0 | SOLA XL | 22.8 | Vis Ease Outlk | 52.0 | AO Compact | 71.9 |
| Rdnstk Life AT | 0.0 | Varlx Panamic | 21.6 | SOLA Percepta | 50.1 | SOLA Percepta | 67.0 |
| Pentx AF Mini | 0.0 | SOLA Percepta | 20.8 | SOLA XL | 48.7 | Shamr Genesis | 63.2 |
| Pentx AF 150 | 0.0 | Pentx AF Mini | 20.2 | Hoya Sum CD | 46.6 | Pentx AF 150 | 62.9 |
| AO b'Active | 0.0 | Ess Adaptar | 19.7 | Sig Kodak | 46.3 | Sig Kodak | 61.4 |
| Shamr Genesis | 0.0 | HoyaLux ECP | 15.5 | AO b'Active | 44.8 | SOLA XL | 61.3 |
| Younger Image | 0.0 | AO b'Active | 14.6 | Ess Adaptar | 43.9 | Ess Adaptar | 60.6 |
| Ess Adaptar | 0.0 | Sig Kodak | 14.1 | Rdnstk Life AT | 43.6 | Vis Ease Outlk | 59.5 |
| Sig Kodak | 0.0 | Rdnstk Life AT | 13.1 | Varlx Panamic | 42.6 | AO b'Active | 58.3 |
| Varlx Comfort | 0.0 | Sig Nav Precsn | 13.0 | Pentx AF Mini | 41.9 | Varlx Panamic | 56.4 |
| Ess Natural | 0.0 | Younger Image | 12.5 | HoyaLux ECP | 41.1 | Rdnstk Life AT | 56.2 |
| Zei Gradal Top | 0.0 | AO Pro 15 | 9.8 | Pentx AF 150 | 41.0 | Zei Gradal Top | 55.6 |
| HoyaLux ECP | 0.0 | Hoya GP Wide | 9.4 | Younger Image | 40.8 | Pentx AF Mini | 54.9 |
| SOLA XL | 0.0 | Pentx AF 150 | 8.7 | AO Pro 15 | 40.0 | AO Pro 15 | 49.5 |
| Sig Nav Precsn | 0.0 | J&J Definity | 5.4 | Zei Gradal Top | 35.0 | Younger Image | 45.3 |
| SOLA Percepta | 0.0 | Ess Natural | 0.0 | J&J Definity | 24.9 | J&J Definity | 12.8 |
| Ess Spr No-lne | 0.0 | Zei Gradal Top | 0.0 | Ess Natural | 20.0 | Ess Natural | 9.8 |
These ratings are useful for those patients for whom near vision is the
single overriding need. Ratings increase with greater fitting heights
commensurate with the greater near viewing zone sizes thereby attained. (Reprinted
with permission of Optometry.)
The ratings in Table 5 combine viewing zones and are based on equal weightings of the distance
and intermediate ratings and the intermediate and near (fitting
height of 22 mm) ratings. The two columns on the left do not consider
the amount of unwanted astigmatism, whereas those on the right include
a 25% weighting of astigmatism. The distance/intermediate
ratings apply to patients with primary visual needs at those two
distances and for whom near viewing is not as important. This includes
drivers or those with outdoor occupations and recreations who have distance
and intermediate viewing needs but for whom near viewing is not
as important. The intermediate and near category applies to patients
who largely work indoors and primarily perform visual tasks at those
viewing distances and for whom distance vision is not as important. The
ratings that include astigmatism weighting apply to patients with sensitivity
to unwanted astigmatism.
TABLE 5. Combination ratings for distance/intermediate,
and for intermediate/near (fitting height of 22 used in rating)
| Specialty usage combinations |
| Without astigmatism weighting | With 25% astigmatism weighting |
| Distance and intermediate | Rating | Intermediate and near (FH 22) | Rating | Distance and intermediate | Rating | Intermediate and Near (FH 22) | Rating |
| Zei Gradal Top | 78.4 | SOLAMax | 75.4 | J&J Definity | 77.4 | SOLAMax | 71.4 |
| Younger Image | 74.2 | Sig Nav Precsn | 68.3 | AO b'Active | 69.2 | J&J Definity | 66.8 |
| J&J Definity | 72.1 | Pentx AF Mini | 64.5 | Younger Image | 69.1 | AO Pro 15 | 64.0 |
| AO b'Active | 72.1 | Rdnstk Life AT | 63.1 | Zei Gradal Top | 68.1 | Rdnstk Life AT | 63.9 |
| Shamr Genesis | 71.3 | Zei Gradal Top | 63.1 | Shamr Genesis | 67.3 | Pentx AF Mini | 63.7 |
| Sig Kodak | 69.1 | HoyaLux ECP | 62.3 | AO Pro 15 | 62.7 | AO b'Active | 60.0 |
| HoyaLux ECP | 65.5 | AO Pro 15 | 62.3 | Sig Kodak | 62.6 | Sig Nav Precsn | 58.7 |
| Vis Ease Outlk | 60.6 | Shamr Piccolo | 60.0 | HoyaLux ECP | 58.0 | Shamr Piccolo | 58.5 |
| AO Pro 15 | 60.5 | AO b'Active | 59.8 | Vis Ease Outlk | 56.0 | Zei Gradal Top | 56.7 |
| SOLA Percepta | 59.4 | Sig Kodak | 58.7 | Varlx Panamic | 54.8 | Shamr Genesis | 56.2 |
| Ess Natural | 57.7 | Hoya GP Wide | 58.5 | Rdnstk Life AT | 54.1 | Varlx Panamic | 56.0 |
| Sig Nav Precsn | 56.9 | Hoya Sum CD | 58.3 | Pentx AF Mini | 54.1 | HoyaLux ECP | 55.6 |
| Pentx AF Mini | 51.7 | J&J Definity | 58.0 | Pentx AF 150 | 53.8 | Hoya Sum CD | 55.6 |
| Pentx AF 150 | 51.3 | Shamr Genesis | 56.5 | Ess Natural | 52.9 | Sig Kodak | 54.8 |
| Rdnstk Life AT | 50.1 | SOLA VIP | 56.0 | SOLA Percepta | 52.0 | Hoya GP Wide | 53.4 |
| Hoya Sum CD | 50.1 | SOLA XL | 55.2 | Sig Nav Precsn | 50.2 | AO Compact | 53.3 |
| Varlx Panamic | 49.7 | Ess Adaptar | 52.9 | Hoya Sum CD | 49.4 | Pentx AF 150 | 52.9 |
| Ess Adaptar | 48.6 | Varlx Panamic | 51.4 | Ess Adaptar | 48.5 | Sig Kod Precise | 52.5 |
| Ess Spr No-lne | 47.0 | Varlx Comfort | 51.2 | SOLAMax | 46.3 | Ess Adaptar | 51.7 |
| SOLA XL | 43.3 | Younger Image | 50.9 | Sig Kod Precise | 45.0 | Younger Image | 51.7 |
| SOLAMax | 41.9 | Pentx AF 150 | 50.1 | Hoya GP Wide | 40.4 | SOLA XL | 49.2 |
| SOLA VIP | 41.9 | Sig Kod Precise | 49.8 | SOLA XL | 40.3 | Rdnstk Life XS | 49.0 |
| Hoya GP Wide | 41.2 | Rdnstk Life XS | 49.7 | Rdnstk Life XS | 39.9 | Varlx Comfort | 48.2 |
| Varlx Comfort | 40.1 | AO Compact | 48.9 | Varlx Comfort | 39.9 | Vis Ease Outlk | 46.5 |
| Sig Kod Precise | 39.8 | Vis Ease Outlk | 48.0 | Shamr Piccolo | 38.4 | SOLA VIP | 44.0 |
| Rdnstk Life XS | 37.7 | SOLA Percepta | 40.4 | AO Compact | 37.5 | Ess Natural | 39.9 |
| Shamr Piccolo | 33.1 | Ess Natural | 40.4 | SOLA VIP | 33.4 | SOLA Percepta | 37.8 |
| AO Compact | 27.7 | Ess Spr No-lne | 37.0 | Ess Spr No-lne | 27.9 | Ess Spr No-lne | 20.4 |
The distance/intermediate ratings apply to patients with primary visual
needs at those 2 distances, near viewing is not factored. The intermediate
and near category applies to patients that primarily perform
visual tasks at those viewing distances and for whom distance vision
is not as important. The ratings that include astigmatism weighting apply
to patients with sensitivity to unwanted astigmatism. (Reprinted
with permission of Optometry.)
The ratings in Table 6 apply for general usage needs. They combine ratings for distance, intermediate, and
near-viewing zones or only distance and near zones; ratings
are provided based on fitting height of both 18 and 22 mm. The
ratings based upon all three zones apply for patients with general
viewing needs at all three distances. If the intermediate viewing zone
is not particularly important to the patient, then the ratings based
on distance and near apply. Unwanted astigmatism is not factored into
the ratings in Table 6. The ratings in Table 7 are the same as in Table 6 except that unwanted astigmatism is factored into the rating. These are
for patients with general viewing needs and for whom reduced astigmatism
is also important.
TABLE 6. General usage combination ratings—no
weighting for unwanted astigmatism
| General usage combinations—no astigmatism weighting |
| Distance, intermediate & near (FH 18) | Rating | Distance, intermediate & near (FH 22) | Rating | Distance and near (FH 18) | Rating | Distance and near (FH 22) | Rating |
| Shamr Genesis | 56.1 | Shamr Genesis | 65.6 | Ess Spr No-lne | 56.5 | Ess Spr No-lne | 73.3 |
| Younger Image | 53.6 | Zei Gradal Top | 63.9 | Shamr Genesis | 54.7 | SOLA Percepta | 69.1 |
| AO b'Active | 52.9 | Younger Image | 63.1 | SOLA Percepta | 54.4 | Shamr Genesis | 68.9 |
| Zei Gradal Top | 52.2 | AO b'Active | 63.0 | Vis Ease Outlk | 53.8 | Vis Ease Outlk | 64.6 |
| Sig Kodak | 50.8 | Sig Kodak | 61.5 | Younger Image | 49.9 | Younger Image | 64.1 |
| Vis Ease Outlk | 50.5 | Vis Ease Outlk | 57.7 | Rdnstk Life XS | 44.0 | SOLA VIP | 62.0 |
| J&J Definity | 49.9 | HoyaLux ECP | 57.4 | SOLA VIP | 43.3 | Rdnstk Life XS | 59.8 |
| HoyaLux ECP | 48.8 | J&J Definity | 56.4 | AO b'Active | 42.0 | AO b'Active | 57.0 |
| SOLA Percepta | 46.5 | SOLA Percepta | 56.3 | Sig Kodak | 40.6 | Sig Kodak | 56.7 |
| AO Pro 15 | 43.6 | Sig Nav Precsn | 55.3 | Shamr Piccolo | 34.1 | Zei Gradal Top | 50.2 |
| Sig Nav Precsn | 42.3 | AO Pro 15 | 53.6 | Sig Kod Precise | 33.0 | Shamr Piccolo | 49.9 |
| Ess Spr No-lne | 41.3 | SOLA VIP | 53.3 | Zei Gradal Top | 32.7 | Sig Kod Precise | 47.3 |
| Pentx AF Mini | 41.2 | SOLAMax | 52.6 | AO Compact | 32.4 | Varlx Comfort | 45.8 |
| Hoya Sum CD | 41.1 | Ess Spr No-lne | 52.4 | HoyaLux ECP | 31.5 | AO Compact | 44.8 |
| SOLA VIP | 40.9 | Rdnstk Life XS | 49.1 | Varlx Comfort | 30.7 | HoyaLux ECP | 44.3 |
| SOLAMax | 40.7 | Hoya Sum CD | 48.9 | Varlx Panamic | 30.4 | Pentx AF 150 | 42.2 |
| Varlx Panamic | 40.3 | Pentx AF Mini | 48.4 | J&J Definity | 29.2 | Hoya GP Wide | 41.8 |
| Ess Adaptar | 39.0 | Rdnstk Life AT | 48.0 | Ess Adaptar | 27.5 | Varlx Panamic | 40.9 |
| Rdnstk Life XS | 38.5 | Pentx AF 150 | 47.9 | Ess Natural | 27.3 | SOLAMax | 40.6 |
| Ess Natural | 38.5 | Shamr Piccolo | 47.7 | Hoya Sum CD | 26.6 | Sig Nav Precsn | 40.6 |
| Rdnstk Life AT | 37.8 | Varlx Panamic | 47.3 | Pentx AF 150 | 26.1 | Ess Adaptar | 39.6 |
| Shamr Piccolo | 37.1 | Hoya GP Wide | 47.2 | SOLA XL | 23.8 | J&J Definity | 39.0 |
| Pentx AF 150 | 37.1 | Ess Adaptar | 47.1 | AO Pro 15 | 23.1 | Hoya Sum CD | 38.4 |
| SOLA XL | 36.4 | Varlx Comfort | 45.7 | SOLAMax | 22.7 | AO Pro 15 | 38.2 |
| Sig Kod Precise | 36.1 | Sig Kod Precise | 45.6 | Sig Nav Precsn | 21.1 | Ess Natural | 37.3 |
| Varlx Comfort | 35.6 | Ess Natural | 45.1 | Pentx AF Mini | 18.2 | SOLA XL | 36.8 |
| AO Compact | 32.2 | SOLA XL | 45.1 | Hoya GP Wide | 17.0 | Rdnstk Life AT | 30.6 |
| Hoya GP Wide | 30.6 | AO Compact | 40.5 | Rdnstk Life AT | 15.3 | Pentx AF Mini | 29.0 |
Distance/intermediate/near ratings useful for patients with general
visual needs, distance/near ratings useful for patients without
intermediate needs. Ratings calculated for fitting height (FH) of 18 and 22, representative of low and high fitting heights, respectively. (Reprinted with permission of Optometry.)
TABLE 7. General usage combination ratings
| General usage combinations—25% astigmatism weighting |
| Distance, intermediate & near (FH 18) | Rating | Distance, Intermediate & near (FH 22) | Rating | Distance and near (FH 18) | Rating | Distance and near (FH 22) | Rating |
| J&J Definity | 60.7 | J&J Definity | 65.6 | Shamr Genesis | 54.8 | Shamr Genesis | 65.5 |
| Shamr Genesis | 55.9 | Shamr Genesis | 63.0 | Younger Image | 50.9 | Younger Image | 61.6 |
| AO b'Active | 54.8 | AO b'Active | 62.4 | Vis Ease Outlk | 50.8 | SOLA Percepta | 59.3 |
| Younger Image | 53.7 | Younger Image | 60.8 | SOLA Percepta | 48.3 | Vis Ease Outlk | 58.9 |
| AO Pro 15 | 50.0 | AO Pro 15 | 57.6 | AO b'Active | 46.6 | AO b'Active | 57.9 |
| Sig Kodak | 48.9 | Zei Gradal Top | 57.3 | J&J Definity | 45.3 | Rdnstk Life XS | 56.5 |
| Zei Gradal Top | 48.5 | Sig Kodak | 56.9 | Rdnstk Life XS | 44.7 | Sig Kodak | 53.4 |
| Vis Ease Outlk | 48.4 | SOLAMax | 54.3 | Sig Kodak | 41.3 | J&J Definity | 52.5 |
| Varlx Panamic | 47.8 | Vis Ease Outlk | 53.8 | AO Compact | 40.9 | Shamr Piccolo | 50.9 |
| Pentx AF Mini | 46.2 | Varlx Panamic | 53.0 | Varlx Panamic | 40.3 | Sig Kod Precise | 50.6 |
| HoyaLux ECP | 45.5 | Rdnstk Life AT | 52.5 | Sig Kod Precise | 39.9 | AO Compact | 50.2 |
| SOLAMax | 45.4 | HoyaLux ECP | 51.9 | Shamr Piccolo | 39.1 | SOLA VIP | 48.5 |
| Rdnstk Life AT | 44.8 | Pentx AF Mini | 51.6 | Ess Spr No-lne | 35.1 | Varlx Panamic | 48.2 |
| Pentx AF 150 | 43.2 | Pentx AF 150 | 51.2 | Pentx AF 150 | 34.9 | Ess Spr No-lne | 47.6 |
| Hoya Sum CD | 42.7 | SOLA Percepta | 49.7 | AO Pro 15 | 34.6 | Pentx AF 150 | 47.0 |
| SOLA Percepta | 42.4 | Sig Kod Precise | 49.4 | SOLA VIP | 34.5 | Zei Gradal Top | 47.0 |
| Sig Kod Precise | 42.2 | Shamr Piccolo | 49.3 | Zei Gradal Top | 33.9 | AO Pro 15 | 46.0 |
| Shamr Piccolo | 41.3 | Sig Nav Precsn | 48.9 | Varlx Comfort | 32.8 | SOLAMax | 45.3 |
| Ess Adaptar | 41.2 | Hoya Sum CD | 48.5 | Ess Adaptar | 32.6 | Varlx Comfort | 44.2 |
| AO Compact | 40.8 | Rdnstk Life XS | 48.5 | HoyaLux ECP | 32.4 | HoyaLux ECP | 42.0 |
| Rdnstk Life XS | 40.6 | Ess Adaptar | 47.3 | SOLAMax | 31.9 | Ess Adaptar | 41.7 |
| Sig Nav Precsn | 39.2 | AO Compact | 47.0 | Hoya Sum CD | 31.8 | Hoya GP Wide | 40.9 |
| Ess Natural | 38.5 | Hoya GP Wide | 44.9 | Ess Natural | 30.2 | Hoya Sum CD | 40.6 |
| Varlx Comfort | 36.5 | Varlx Comfort | 44.1 | Pentx AF Mini | 29.0 | Rdnstk Life AT | 39.5 |
| SOLA XL | 35.2 | Ess Natural | 43.5 | Rdnstk Life AT | 28.0 | Sig Nav Precsn | 37.9 |
| SOLA VIP | 32.6 | SOLA VIP | 42.0 | SOLA XL | 25.7 | Ess Natural | 37.6 |
| Hoya GP Wide | 32.4 | SOLA XL | 41.6 | Sig Nav Precsn | 23.3 | Pentx AF Mini | 37.1 |
| Ess Spr No-lne | 23.6 | Ess Spr No-lne | 32.0 | Hoya GP Wide | 22.2 | SOLA XL | 35.4 |
Same as Table 4 but with 25% weighting for unwanted astigmatism. Same
use as Table 4 but for patients with sensitivity to unwanted astigmatism. (Reprinted
with permission of Optometry.)
FITTING PROGRESSIVE ADDITION LENSES Both the vertical and horizontal positioning of the PAL within the eye
of the frame are critical. Because the near addition in a PAL is relatively
low in the lens, a frame with a relatively large B (vertical) dimension
should be selected, preferably larger than 30 mm. Frames
with adjustable nose pads are also advisable, to enable postdispensing
adjustment of the location of the lenses before the eyes. The frame
must be properly adjusted to include pantoscopic angle, vertex distance, and
vertical wearing position prior to measuring the lens location. PALs are designed to have the fitting cross placed directly in front of
the pupil with normal straight-ahead gaze. For each design this
provides the optimal location of the viewing zones and the optimal binocular
use of the lenses. The vertical height of the fitting cross should
be measured from the pupil down to the lowest edge of the lens in
the frame. The ratings in Table 4 show that considerably greater near
areas and widths are attained with greater fitting heights. Only a few
PALs provide a near-viewing zone with a fitting height of 16, and
a fitting height of 22 provides considerably greater near zone than
a fitting height of 18 for all of the lenses. Small frames, which
result in shorter fitting heights, require careful selection of PAL design (far
left columns of Table 2). Even with a properly selected short-corridor PAL, fitting heights
shorter than 18 necessarily result in some compromise of the near-viewing
zone and the patient should be advised of such. The compromised
near zone will be noticeable in conditions of low illumination (menu
in a restaurant) because of a larger pupil, high reading
demands (office work or reading a book in the evening), or
viewing small print (phone book). Many patients consider these
as reasonable trade-offs for the fashionable small frame. Separate
reading glasses or OPLs can be prescribed for specific near-viewing
tasks. Accurate measurement of the PD is particularly critical for successful
wearing of a PAL. This is because of the narrowness of the intermediate
channel that is directly below the fitting cross. The narrowest portion
of the average PAL (Fig. 6) is approximately 3 mm, or about the same size as the pupil of the
eye. If the pupils of both eyes are to be able to simultaneously view
through the channel, there is essentially no tolerance for error in
the separation of the two lenses. Any error in the separation of the lenses
relative to the PD of the patient results in one of the eyes viewing
through an edge of the channel when the other is centered in it. Improper
measurement of PD may be the largest reason for patient nonacceptance
of PALs. PD measurement with a pupillometer is probably the most accurate method. Accurate
measurement of the total PD is the most important, however, it
is also advisable to specify the split, or monocular components of
the PD as enabled by a pupillometer. ADAPTATION TO PALS Some patients have difficulty adapting to PALs. However, this problem has
lessened considerably with newer designs and the high acceptance rates
of PALs indicate this problem is becoming uncommon. Adaptation problems
can be related to spatial distortion resultant from the pattern
of unwanted astigmatism in the lower quadrants of the lens. Such patients
will report swimming sensations, spatial disorientation, warped appearance
of lines, or vague complaints. Other patients may have difficulty
with the width of the distance, intermediate, or near-viewing
zones. Distortion is less and zones are wider for lower adds, therefore, adaptation
is easiest for the beginning presbyope. Adaptation to
a PAL will be more difficult for a first-time wearer with a higher
add. As with most spectacle lens adaptation, it may take up to 2 weeks
of continuous wear for adaptation. Adaptation difficulties can often be managed by adjusting the pantoscopic
angle, the vertex distance, or the fitting height (if the frame
has adjustable nose pads). Verify that the distance between lens
centers matches the patient's PD; mismatch can certainly cause adaptation
problems. If the patient difficulties concern the width or area
of one of the viewing zones, consult Tables 3 through 7 to determine if
the complaints match the lens characteristics and whether another PAL
design would resolve the problem. If the problems cannot be resolved, common
industry practice is to replace the PAL lenses with bifocals
with no additional charge to doctor or patient. |