|
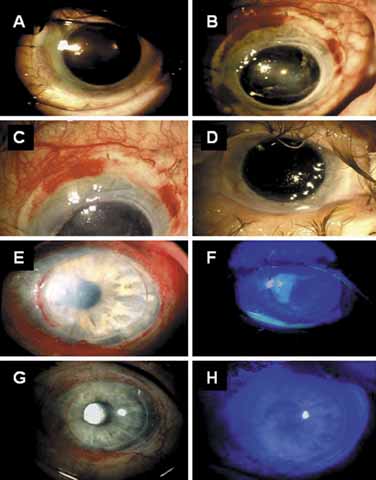
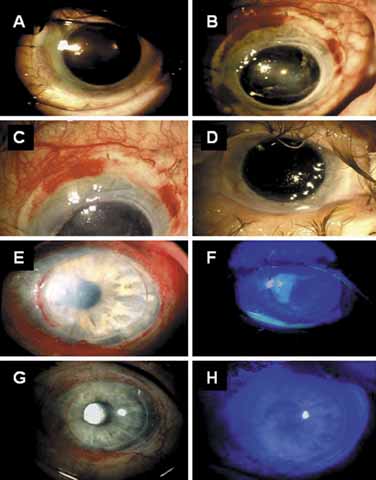
| Fig. 9 Allograft rejection of keratolimbal allograft transplant (KLAL) and management. A. A 77-year-old male underwent KLAL elsewhere and was treated with mycophelonate (CellCept®) 1 g/d. B and C. He presented on a routine follow-up visit with perilimbal redness, vessel engorgement with hemorrhage, and progressive ulceration. D. Postoperative view of a quiescent eye after a repeat penetrating keratoplasty (PKP) and institution of mycophelonate, prednisone and cyclosporine using the regimen described in Table 2. E. A 22-year-old male with chemical burn received KLAL elsewhere and presented with reduced vision, redness, and photophobia while under oral mycophelonate alone. He was noted to have vessel engorgement and ulceration with a 3 × 4 mm corneal epithelial defect (see inset). F. Impression cytology showed lymphocyte infiltration at the border of ulceration (see arrows) and no conjunctivalization, supporting the diagnosis of immune rejection and not total limbal stem cell deficiency (LSCD). Lymphocyte infiltration 100× magnification (inset). G and H. Two weeks after addition of cyclosporine and prednisone, the limbal inflammation and redness was reduced and the ulceration ceased. (Modified from Espana EM, Di Pascuale M, Grueterich M, et al: Keratolimbal allograft for corneal surface reconstruction. Eye 110:481, 2003, with permission) |