

|
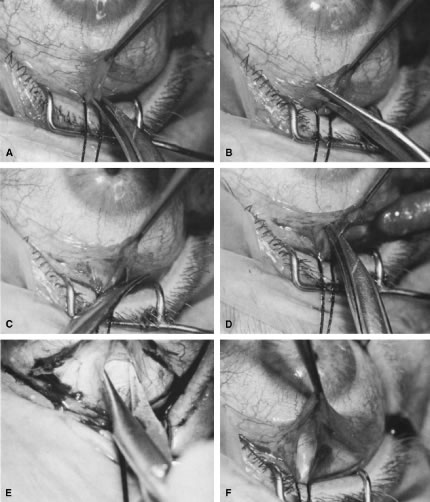
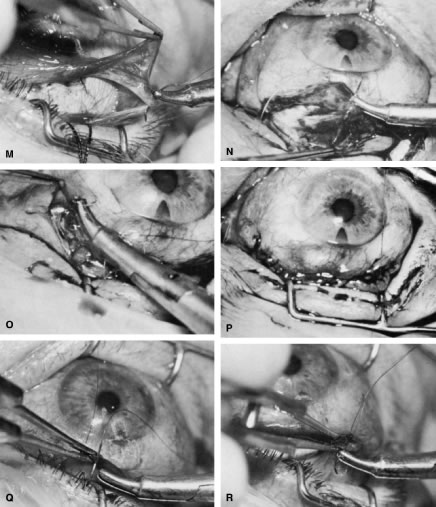
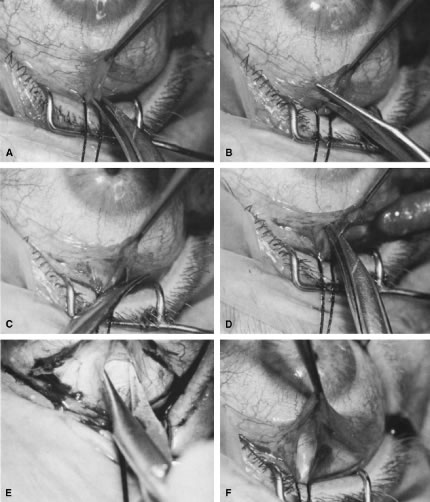
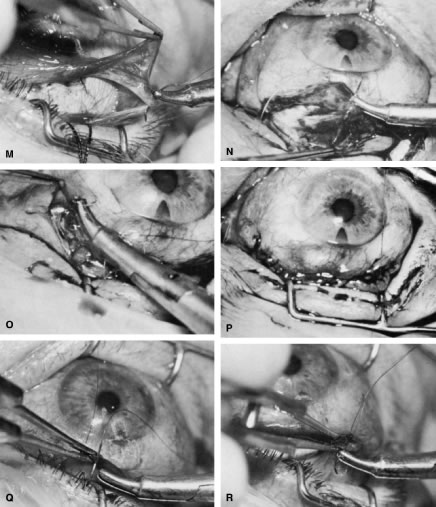
| Fig. 13. Limbus-based flap procedure. A. Conjunctiva is lifted away from the globe, stretched, and incised adjacent to the superior rectus muscle bridle suture. B. The incision in the conjunctiva is extended nasally. C. The conjunctival incision is extended temporally. D. Tenon's capsule is lifted up, away from the globe, and incised with the scissors held obliquely to avoid cutting into the underlying superior rectus muscle. E. The incision in Tenon's capsule is spread bluntly. F. The superior rectus muscle can be seen through the buttonhole in Tenon's capsule. Bleeding should be minimal; if it occurs, it should be controlled promptly with cautery. G. Tenon's capsule is incised nasally and temporally. H. The connective tissue overlying the superior rectus muscle is seen easily after Tenon's capsule has been incised. This tissue usually is highly vascular in the area directly at the base of the superior rectus muscle. I. Episclera is buttonholed approximately 4 mm posterior to the limbus, showing the underlying sclera. J. One blade of the scissors is insinuated between the sclera and the episclera, and the episclera is incised nasally. K. The episclera is incised temporally. The plane of the scissors is flush with the sclera. L. Remaining adhesions between the episclera and sclera are dissected in a semisharp fashion with the no. 67 Beaver blade, which is pushed at right angles to the cutting axis. M. Tenon's capsule is closed in a separate layer with an 8-0 absorbable suture. N. The superior edge of Tenon's capsule tends to retract up under the lid. It can be hooked over the needle and pulled inferiorly. Sutures are locked. O. After Tenon's capsule is closed, the needle is placed from the underneath side to the superficial side of the conjunctiva and exteriorized so that it can be used to close the conjunctiva. P. The conjunctiva is closed with closely spaced running, unlocked sutures. The final suture is tied securely. Q. After the needle has passed through the tissue, it is lifted away from the globe firmly. The underlying tissue is stretched. A blunt forceps is used to grasp this underlying tissue firmly, as close to the needle as possible. This maneuver will hold the needle firmly in place, permitting the surgeon to release the end of the needle containing the suture without having to change the position of the needle. R. The needle can be regrasped toward the cutting end so that it is held in proper position for placement of the next suture. (Spaeth GL. Glaucoma surgery. In Spaeth GL (ed). Ophthalmic Surgery: Principles and Practice. Philadelphia: WB Saunders, 1990.) |